Correlation Between Lymphedema Disease Severity and Lymphoscintigraphic Findings: A Clinical-Radiological Study
Reid A. Maclellan, M.D., M.M.Sc, David Zurakowski, PhD, Stephan Voss, MD, PhD, Arin K. Greene, MD, MMSc.
Children's Hospital Boston / Harvard Medical School, Boston, MA, USA.
Background: Lymphoscintigraphy is used to confirm the diagnosis of lymphedema; pathological findings are abnormal transit time to regional nodes and dermal backflow. A universal protocol for the test does not exist. The purpose of this study was to determine if the clinical severity of lymphedema correlates with lymphoscintigraphy findings.
Methods: Patients treated in our Lymphedema Program between 2009 and 2017 were reviewed. Diagnosis of lymphedema was determined by history, physical examination, and lymphoscintigraphy. Severity was defined by increased volume of the limb: mild (<20%), moderate (20-40%), severe (>40%). Candidate variables included location (arm, leg), age, duration of symptoms, infection history, and lymphedema type (primary, secondary). An association between lymphedema severity and lymphoscintigraphy findings was determined using the Pearson chi-square test and multivariate logistic regression.
Results: One hundred thirty-four patients with 181 affected extremities (24 upper, 157 lower) were included. Clinical severity was: 54% mild, 30% moderate, and 16% severe. Delayed tracer transit to the regional nodes was: 45 minutes (34%), 2 hours (18%), and ≥ 4 hours (48%). Thirty-six percent of extremities demonstrated dermal backflow. Abnormal transit time or dermal backflow was identified in 97% of extremities by 45 minutes and in 3% of limbs by 2 hours. Transit time and dermal backflow were not predictive of clinical severity when adjusting for candidate variables (p > 0.1).
Conclusions: Clinical severity of lymphedema is not associated with lymphoscintigraphy findings. A lymphoscintigram should be interpreted as normal or abnormal, and does not need to exceed 2 hours.
Figure: Correlation of transit time and dermal backflow with lymphedema severity. (Top, Left) 40 year-old male with severe lymphedema of the right lower extremity (>40% volume increase) with decreased, but visible tracer uptake in right inguinal nodes (arrowhead) 2 hours following injection of radionuclide. (Top, Right) 15 year-old female with mild disease (<20% volume increase) and no transit to the right inguinal nodes (arrowhead) 4 hours after radionuclide administration. (Bottom, Left) Dermal backflow is absent in 65 year-old male with severe disease. (Bottom, Right) 29 year-old male with severe lymphedema and dermal backflow (arrow). 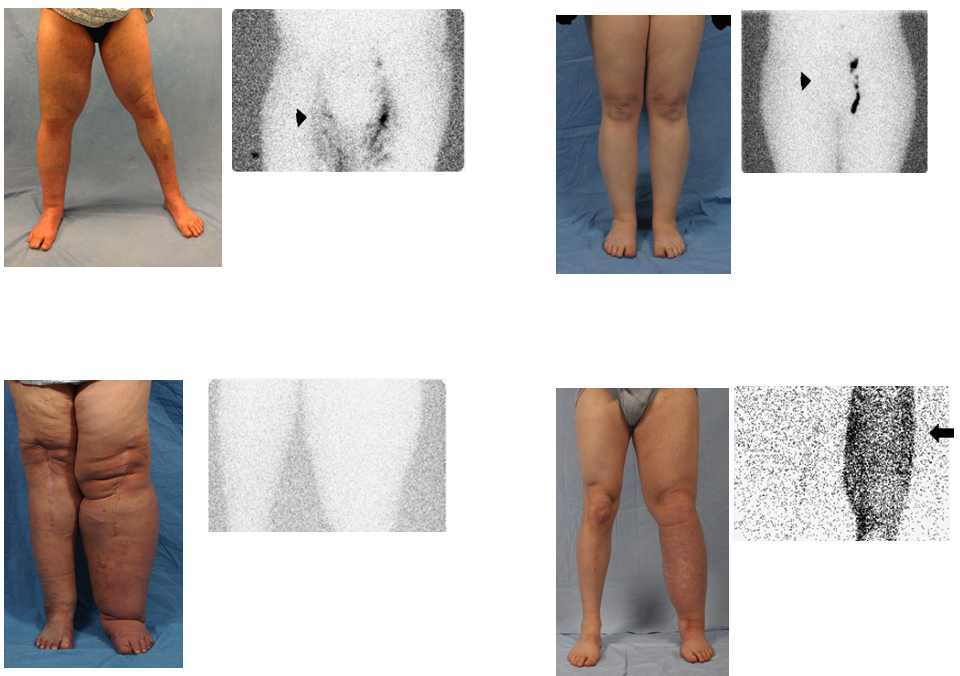
Back to 2017 Program




