Benefit on Lymphedema after Delayed Breast Reconstruction
Charalampos Siotos, MD, Aladdin H. Hassanein, MD, MMSC, Ricardo J. Bello, MPH, Mohamad E. Sebai, MBBS, Stella M. Seal, MLS, Carisa M. Cooney, MPH, Gedge D. Rosson, MD.
Johns Hopkins University, Baltimore, MD, USA.
BACKGROUND: Breast-cancer-related-lymphedema (BCRL) is a debilitating condition with morbidity, hindered quality of life and increased health-related costs. Experimental studies support the use of musculocutaneous flaps for managing animal models with lymphedema. Although vascularized lymph node transfer and lymphovenous anastomosis (LVA) are used to surgically treat patients with lymphedema, it is unknown whether musculocutaneous flaps (i.e., delayed autologous breast reconstruction) are effective for treating refractory upper extremity BRCL. We conducted a systematic review and pooled analysis to assess the impact of delayed breast reconstruction on established BCRL.
METHODS: Following (PRISMA) guidelines, we systematically searched PubMed, Scopus, Embase and Goolge Scholar databases for relevant studies published from inception through November 11, 2016. No language restrictions were employed. Articles assessing lymphedema response to delayed autologous breast reconstruction were included. We screened 853 unique articles based on title and abstract. Of these, we conducted full text and reference screening on 37 articles. We performed a pooled analysis using random effects to quantitively synthesize results from individual studies.
RESULTS:Eight studies met inclusion criteria for our systematic review. One study was a case report; seven studies were case series with sample sizes ranging from three to thirty-eight patients. Patients that received breast reconstruction with or without lymph node transfer were more likely to report improved than stable or deteriorated lymphedema by 64% (p<0.05). Pooled analysis (Figure) demonstrated that studies describing breast reconstruction including lymph node transfer as part of the procedure reported significantly higher rates of improvement of lymphedema (percent of patients improved=0.84 95%CI=0.74-0.95, p<0.05) compared to studies that reported on patients undergoing breast reconstruction without lymph node transfer (percent of patients improved=0.22, 95% CI=0.12-0.32, p<0.05).
CONCLUSIONS: Our review is the first that summarizes the current evidence that delayed autologous breast reconstruction may be a sufficient treatment for breast-cancer-related-lymphedema. Further clinical studies are warranted investigating the necessity of vascularized lymph node transfer/LVA in patients with BCRL undergoing delayed breast reconstruction. 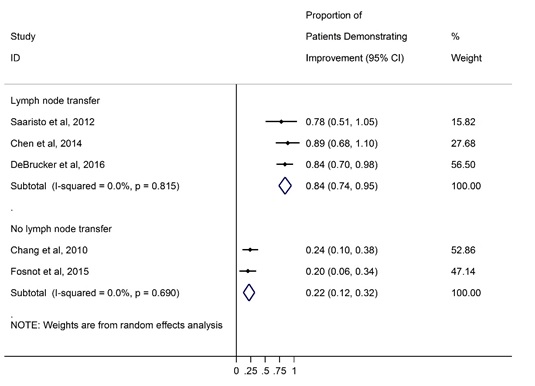
Back to 2017 Program




