Single-Center Evaluation of Prophylactic Mastectomy and Reconstruction Outcomes: The Benefits of Autologous Reconstruction
Patrick P. Bletsis, BSc, Alexandra Bucknor, MBBS, MRCS, MSc, Anmol Chatta, BA, Austin Chen, Bernard Lee, MD, MPH, FACS, Samuel Lin, MD, MBA, FACS.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
A Single-Center Evaluation of Prophylactic Mastectomy and Reconstruction Outcomes: The Benefit of Autologous Reconstructions
Patrick Bletsis, BSc, 1 Alexandra Bucknor, MBBS, MRCS, MSc,1 Anmol Chattha, BA1 Austin Chen, BA,1 Bernard T. Lee, MD, MPH, FACS,1 Samuel J. Lin, MD, MBA, FACS1
1Division of Plastic and Reconstructive Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
Background
Over the last decade, we have seen a 12% increase in prophylactic mastectomies (PM) annually. Indications for PM vary and include genetic predisposition or strong family history. At our institution, autologous flap reconstruction is the favored method of post-mastectomy breast reconstruction. However, evidence suggests that rates of PM and breast reconstruction modality varies between institutions; it is, therefore, important to evaluate the complication profile associated with different reconstructive modalities in this patient group. In this study, we reviewed post-operative outcomes in women undergoing PM and breast reconstruction at our institution.
Methods
A retrospective chart review of consecutive women undergoing a contralateral (CPM) or bilateral (BPM) PM between 2010 and 2015 at a single academic institution was performed. Patients with malignancy on final pathology were excluded. Patient demographics, comorbidities, type of mastectomy and reconstruction, intraoperative and postoperative outcomes were collected and analyzed. Reconstructions involving combined latissimus dorsi flaps and implants were included in the prosthetic cohort. Postoperative complications were grouped into two categories (minor and major) using the Dindo Classification for surgical complications. Patients undergoing all types of reconstructions were included in the univariate and multivariate model. Models were built looking at both independent risk factors for minor and major complications. P < 0.05 was considered significant for inclusion into multivariate model.
Results
We identified 314 women (417 breasts) that underwent reconstruction after PM during the five-year study period; 171 women (214 breasts) underwent autologous reconstruction and 143 women (176 breasts) underwent prosthetic reconstruction. Patients undergoing PM had an average mean follow up time was 39.4 months, average age of 48.7 years and the average BMI was 27.6 kg/m2. The overall complication rate was 15.9%. Women having an autologous reconstruction had a lower incidence of minor complications (11.2% vs. 18.8%, p=0.036), breast seroma (2.3% vs. 7.4%, p=0.018) and breast infection (1.9% vs. 13.1%, p<0.001) when compared with prosthetic reconstruction (see table 1). Risk factors for minor or major complications included: age (≥65), obesity, ASA class (≥3), smoking, hypertension, anxiety, tissue expander (+ADM), and implant-only reconstructions.
Conclusion
Prophylactic mastectomy and reconstruction rates are rising and represent an important component of the management of women with a high risk of developing breast cancer. In our study, autologous reconstruction had a better complication profile than prosthetic reconstruction. Clinicians can use this information to aid pre-operative counselling of women considering prophylactic mastectomy and reconstruction.
Word count 390
Table 1: comparison of outcomes between autologous and prosthetic breast reconstruction 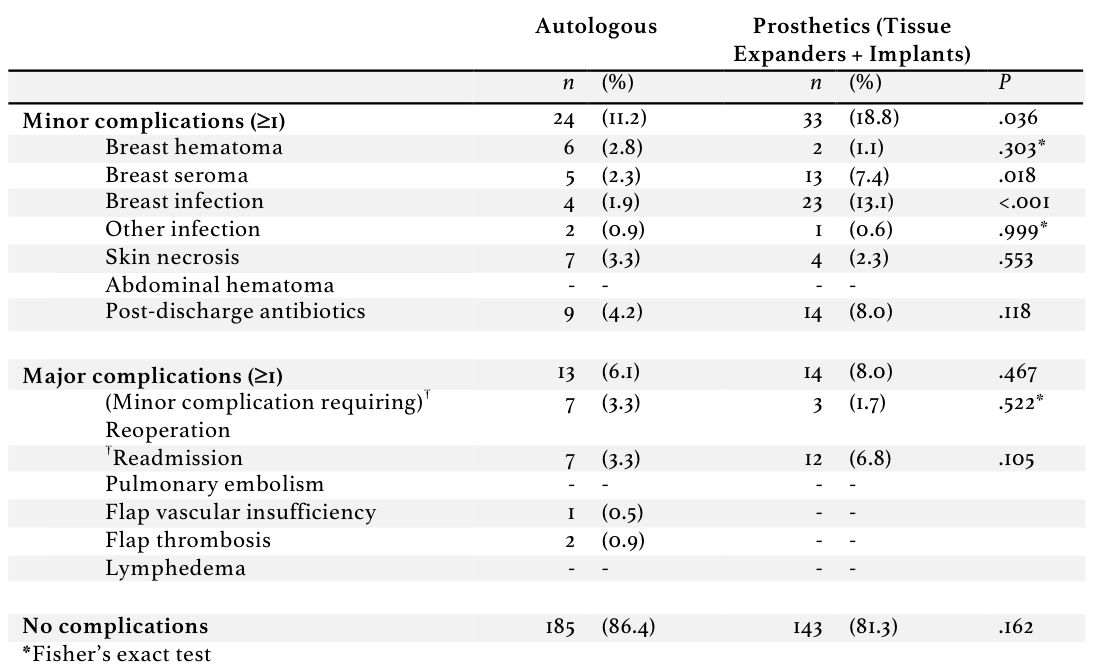
Back to 2017 Program




