Evaluating Reconstructive Outcomes with Immediate, Permanent Implant Reconstruction after Unilateral Nipple-Sparing Mastectomy
Jordan D. Frey, MD, Ara A. Salibian, M.D., Mihye Choi, M.D., Nolan S. Karp, M.D..
NYU Langone Medical Center, New York, NY, USA.
Background:
Nipple-sparing mastectomy (NSM) with immediate, permanent implant reconstruction can achieve excellent results in a single-stage. Outcomes, including ability to achieve symmetry with the contralateral breast, have not yet been established and compared in unilateral reconstructions.
Methods:
Patients undergoing NSM with unilateral immediate, permanent implant reconstruction were reviewed and compared to bilateral reconstruction.
Results:
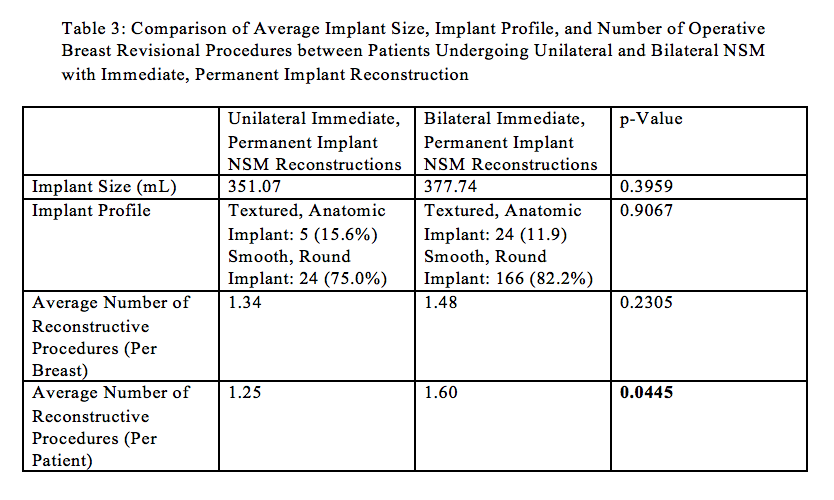
Of 1037 NSMs, 234 (22.6%) underwent immediate, permanent implant reconstruction. Thirty-two patients (13.7%) underwent immediate, permanent implant reconstruction after unilateral NSM. Average age and BMI were 51.47 years and 22.47 kg/m2. Approximately 84% of patients underwent NSM for a therapeutic indication; 8 (25%) patients had a contralateral cancer reconstructed. Of these, 7 patients (21.9%) had a prior contralateral cancer reconstructed and one patient (3.1%) underwent a simultaneous, contralateral tissue expander-based breast reconstruction. The majority (75.0%) of reconstructions utilized smooth, round implants; 15.6% utilized textured, anatomic implants. Acellular dermal matrices were utilized in 78.1% of patients. Average implant size was 351.07 mL. Average follow-up time was 27.39 months.
The most common reconstructive complications were partial nipple necrosis (15.6%) and minor mastectomy flap necrosis (9.4%) followed by major mastectomy flap necrosis and hematoma (3.1%, each). There were no instances of complete nipple necrosis, explantation, or reconstructive failure.
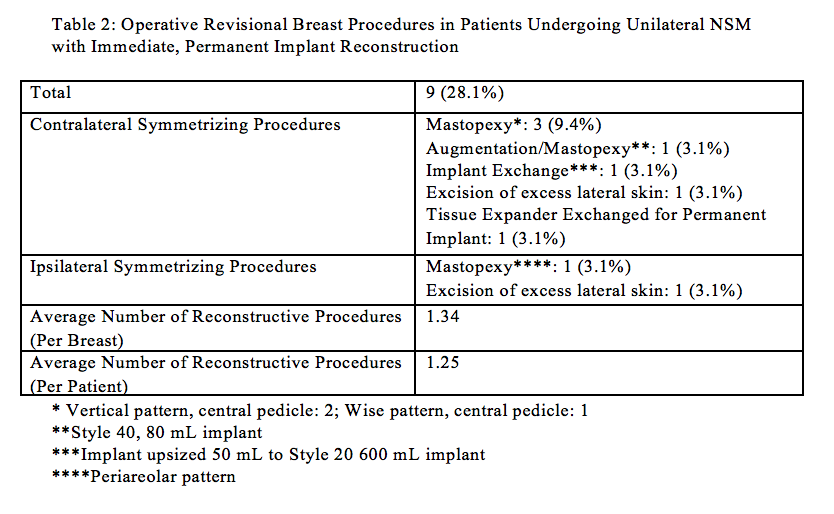
Nine patients (28.1%) underwent subsequent operative breast revisional procedures. Contralateral symmetrizing procedures were undertaken in 21.9%; 6.3% underwent ipsilateral symmetrizing procedures. Revisional procedures included ipsilateral or contralateral mastopexy (12.5%), excision of excess lateral skin (6.3%), augmentation/mastopexy, implant exchange, and tissue expander for implant exchange (3.1%, each). Contralateral symmetrizing procedures were performed in 40% (2/5) of patients who underwent contralateral breast reconstruction. The average number of reconstructive procedures per breast and per patient were 1.34 and 1.25, respectively.
Compared to bilateral NSM with immediate, permanent implant reconstruction, there was no significant difference in terms of implant size (p=0.3959) or implant profile (p=0.9067). When revisional procedures were compared on a per breast basis, there was no significant difference between unilateral and bilateral reconstructions (p=0.2305). When compared on a per patient basis, patients with unilateral single-stage implant NSM reconstruction were found to undergo significantly less revisional procedures compared to bilateral reconstructions (p=0.0445).
Conclusions:
Immediate, permanent implant reconstruction after unilateral NSM achieves excellent results in a single-stage without needing additional reconstructive procedures in the majority of cases. 
Back to 2017 Program




