Physician Payment Trends and Price Variations for Methods of Immediate Breast Reconstruction: A Claim-based Analysis
Hina Panchal, MD MPH1, Clifford Sheckter, MD2, Shantanu N. Razdan, MD MSPH1, Day Yi, MS1, Peter G. Cordeiro, MD1, Joseph J. Disa, MD1, Babak Mehrara, MD1, Evan Matros, MD MMSc. MPH1.
1Memorial Sloan Kettering Cancer Center, New York, NY, USA, 2Stanford University School of Medicine, Stanford, CA, USA.
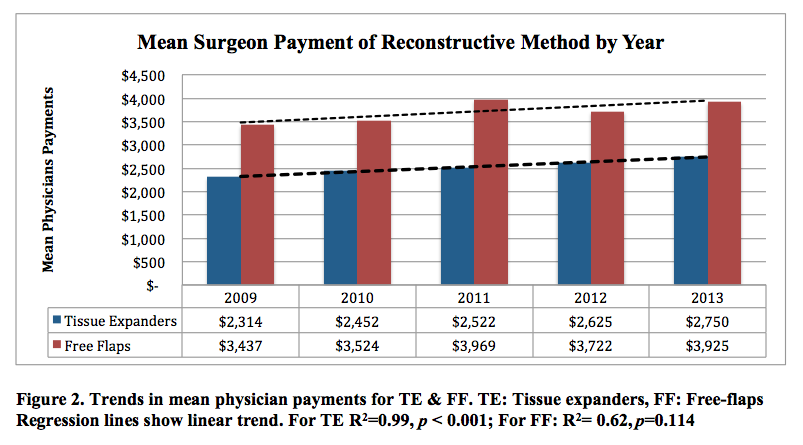
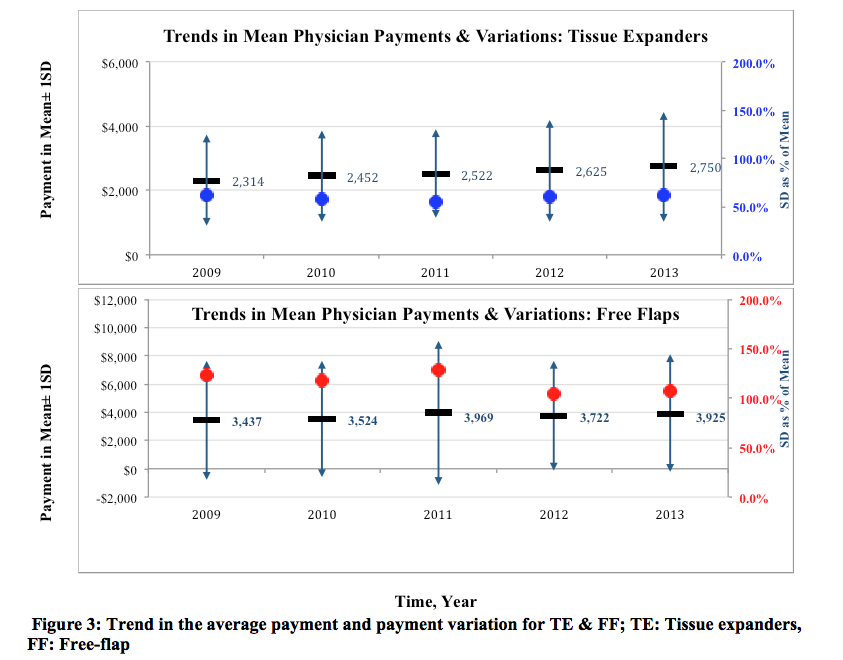
Background: Breast reconstruction has steadily increased in the U.S. over the past two decades with a notable rise in rates of prosthetic reconstruction with stagnation in autologous techniques. Physician payment relative to the effort required for autologous reconstruction has been reported as one barrier underlying these trends. Single institution data suggest that physician reimbursement for prosthetic reconstruction has increased, while for autologous reconstruction it has plateaued. No national claims analysis of plastic surgeon payment for the common methods of breast reconstruction exists. The study aim is to assess national payment trends and price variation for immediate breast reconstruction(IBR) methods: tissue expanders (TE) and free flaps (FF). The hypothesis is that there is increasing payment disparities between tissue expanders and free flaps. Methods: The Blue Health Intelligence (Blue Cross/Blue Shield), a national claim-based database, was queried retrospectively for the period of 2009-2013. Women aged 18 and older with claims for immediate breast reconstruction after mastectomy for breast cancer were included in the study. Trends and variations in the volume of surgery and physician reimbursement were analyzed by procedure type and year. Reimbursement variation was demonstrated by the coefficient of variation (CV), standard deviation as a percentage of the mean payment. Longitudinal trends were assessed with linear regression. Results: 25,209 women underwent IBR in the five-year period, with a significant overall rise in TE (p=0.002) and non-significant rise in FF volumes (p=0.055). Stratifying by laterality, only bilateral TE had a significant rise in volume (p=0.008) whereas unilateral TE and bilateral FF increased, but at non-significant levels (Figure 1). In contrast, unilateral FF saw a significant decline in procedural volume (p=0.042). Mean physician payments increased for both TE and FF, but only the rise in TE payments was statistically significant (p<0.001;Figure 2). There was substantially greater payment variation, as expressed by the coefficient of variation, for FF than TE (CV= 116%vs.59%; Figure 3). Conclusion: IBR volume continues to rise with a significant increase in bilateral TE and a decline in unilateral FF. Payments associated with TEs are rising while payments for FF have stagnated. One interpretation is that these payment trends reflect greater demand by patients for prosthetic techniques. Alternatively, the opportunity cost of performing autologous transfer may not be worthwhile for physicians leading to a relative decline in number of these procedures. The greater variation in physician payments for FF compared to TE suggests greater potential room for negotiation with insurers. Further investigations exploring possible economic drivers in association with reconstructive trends are needed to ensure women have equal access to their desired method of breast reconstruction. 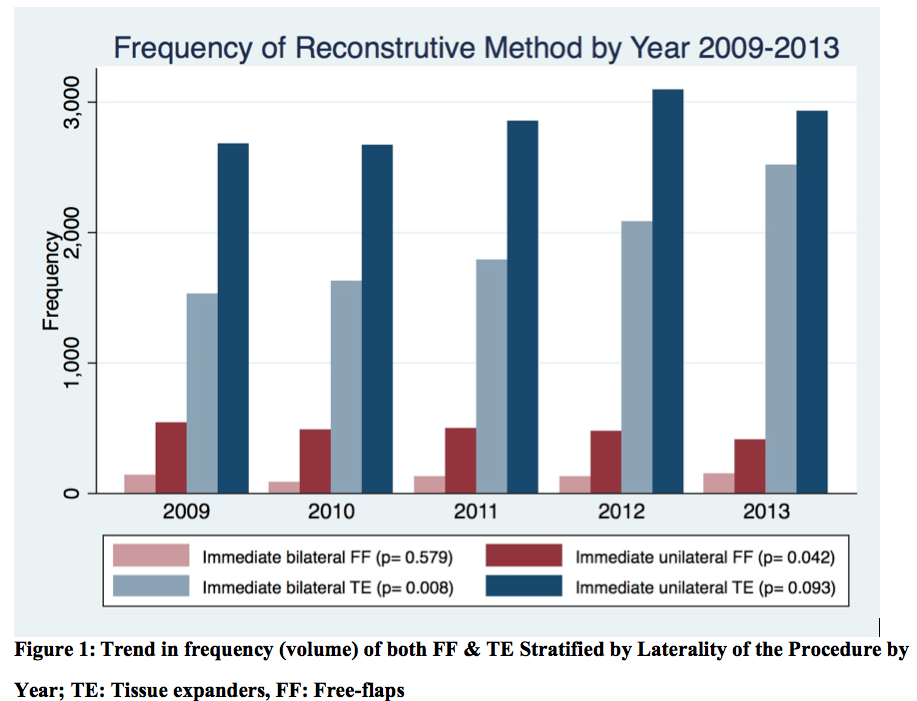
Back to 2017 Program




