Novel Application of Thermal Imaging for Free Flap Harvest and Monitoring
Morgan Brgoch, MD, Logan Carr, MD, Dino Ravnic, DO, T Shane Johnson, MD.
Penn State Hershey Medical Center, Hershey, PA, USA.
Background: Thermal imaging devices such as the FLIR ONETM (FLIR Systems, Wilsonville, Oregon) captures and displays the infrared radiation (IR) emitted from an object. This enables the observer to visually distinguish small temperature differences or temperature variation over time. Although the technology is still evolving, surgical application for identification of perforators has been proposed. In combination with a compatible smartphone, thermal imaging may be used to monitor the relative tissue perfusion rapidly with little training. In this study, we aim to determine the clinical utility of thermal imaging in the perioperative setting.
Methods: Perioperative thermal imaging and standard photographs were taken for 15 patients who underwent free tissue transfer. Intraoperative and post operative utilization of thermal imaging was added to our standardized free flap monitoring protocol, which includes hourly nursing evaluation and Doppler exam, with physician examination every six hours. Both doppler tones and thermal imagining were continued a minimum of 48 hours post operatively. In addition to standard patient demographics post operative outcomes included: Incidence of partial or complete flap loss, arterial or venous insufficiency, reoperation, hematoma, seroma, surgical site infection, or wound dehiscence.
Results: Free flaps utilized for reconstruction include: Free Fibula Osteocutaneous Flap (1), Anterolateral Thigh (ALT) Fasciocutaneous Flap (1), Muscle-Sparing Transverus Abdominus Myocutaneous (msTRAM) (6) and Deep Inferior Epigastric Perforator (DIEP) Flaps (7). One patient experienced unilateral DIEP flap arterial insufficiency. Despite persistent doppler tones in the affected flap, the insufficiency was perceptible with thermal imaging and confirmed with serial physical exams. This flap was subsequently debrided. No other complications were noted; no false positives were found.
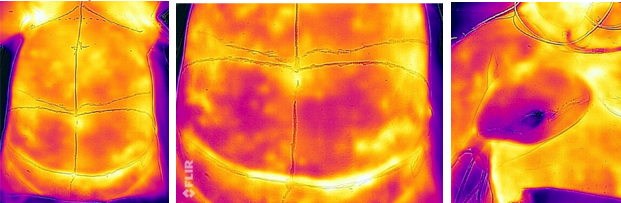
Figure 1 - Preoperative Identification of perforating vessels and subsequent post-operative imaging noting arterial insufficiency and partial flap loss.
Conclusion: Current evaluation of flap perfusion has been limited to intraoperative angiography or other cost prohibitive post-operative monitoring devices. Despite extensive testing, no device has proven significantly advantageous over physical exam in determining post operative flap viability. In this series, thermal imaging (i.e. FLIR ONETM) provides a low cost alternative to visually monitor relative flap perfusion and performed better at identifying arterial insufficiency than bedside doppler exams.
Back to 2017 Program




