Smoking as an Independent Risk Factor for Postoperative Complications in Plastic Surgical Procedures; A Propensity-Matched Analysis of 36,454 Patients from the NSQIP Database from 2005-2014
Yoshiko Toyoda, BA1, Rose Fu, MD1, Lu Li, MS1, David Ottberburn, MD, FACS1, Christine Rohde, MD, MPH, FACS2.
1Weill Cornell Medical Center, New York, NY, USA, 2Columbia University Medical Center, New York, NY, USA.
Background
Smoking has been associated with increased wound healing complications and overall morbidity in multiple specialties, including plastic surgery. From 2005-2014, the smoking rate among U.S. adults decreased from 20.9% to 16.8%. This study aims to investigate (1) whether smoking prevalence in the plastic surgery patient population paralleled the declining national trend and (2) whether smoking remained an independent risk factor for perioperative complications after propensity matching for demographics and other comorbidities.
Methods
The 2005-2014 American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was used to examine smoking prevalence and 30-day postoperative complications in patients who underwent common plastic surgical procedures where extensive planes of dissection make wound healing a greater concern. This was compared to the national smoking incidence. Patients were propensity matched for demographics and comorbidities to isolate smoking as a risk factor. Smokers were further analyzed based on number of pack-years.
Results
We examined 36,454 patients from the 2005-2014 NSQIP database who underwent the following procedures: abdominoplasty, panniculectomy, breast reduction, breast reconstruction with free flap, pedicled muscle flap, or tissue expander, and mastopexy. Overall, a significantly smaller percentage of plastic surgical patients were smokers compared to the corresponding annual national average with a less dramatic decline in smoking incidence than the national trend (p=0.01). There was a bimodal age distribution of smokers in the plastic surgical patient population, and smokers were generally more comorbid than were non-smokers. After propensity score matching, smokers and nonsmokers did not differ significantly in preoperative variables. Smokers continued to have significantly higher rates of deep surgical site infections (SSI) (p<0.01), incisional dehiscence (p<0.01), and need for reoperation (p<0.01). However, incidences of superficial SSI were not significantly different between smokers and nonsmokers (p=0.18). Smokers with ≥11 pack-years were significantly more likely to suffer deep SSI and require reoperation (p<0.01). Additionally, there were no significant differences in incidence of graft/flap loss (p=0.07), bleeding (p=0.40), sepsis (p=0.87) or venous thromboembolic frequency (p=0.16) between smokers and non-smokers (Table).
Conclusions
This study is the first large-scale database analysis isolating smoking as a risk factor for postoperative complications in plastic surgical procedures. Propensity score matching ensures a more uniform comparative cohort in an effort to eliminate confounders and bias. Our data suggests smoking to be an independent risk factor for serious deep SSI, incisional dehiscence, and need for reoperation. Interestingly, superficial SSI rates were not significantly different which may be either a true finding or a result of report bias, which is a limitation in this retrospective analysis. We recommend continued judicious
patient selection and careful preoperative counseling about smoking in order to optimize postoperative patient outcomes and satisfaction. 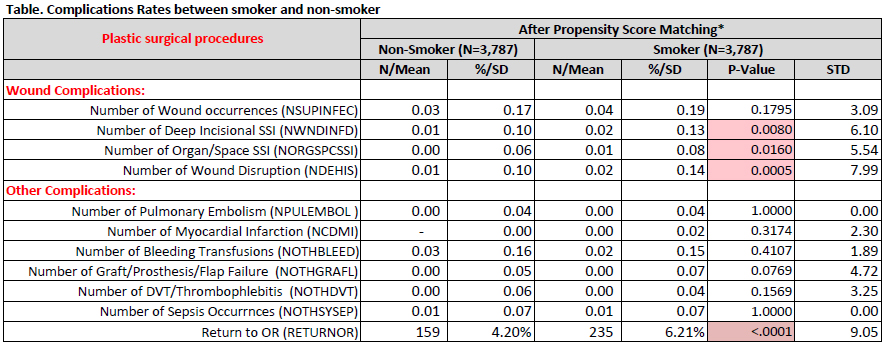
Back to 2017 Program




