Outcomes with Tissue Expander, Immediate Implant, and Autologous Reconstruction in Greater than 1000 Nipple-Sparing Mastectomies
Jordan D. Frey, MD, Ara A. Salibian, M.D., Mihye Choi, M.D., Nolan S. Karp, M.D..
NYU Langone Medical Center, New York, NY, USA.
Background:
Nipple-sparing mastectomy (NSM) permits complete preservation of the nipple-areola complex. Outcomes in NSM have not been directly compared for tissue expander (TE)-, immediate implant-, and autologous-based breast reconstruction after NSM.
Methods:
All patients undergoing NSM from 2006 to June 2016 were identified at a single institution. Demographics and outcomes were analyzed and compared among three breast reconstruction techniques.
Results:
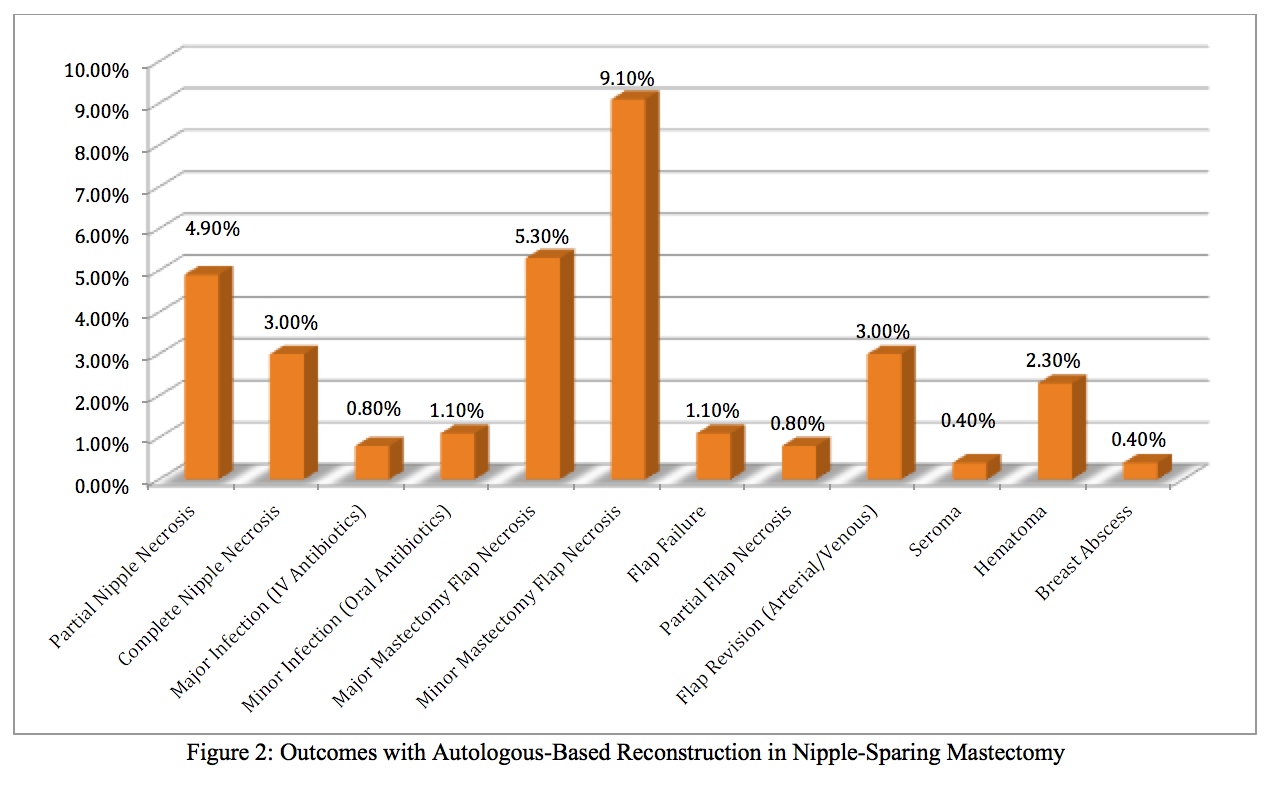
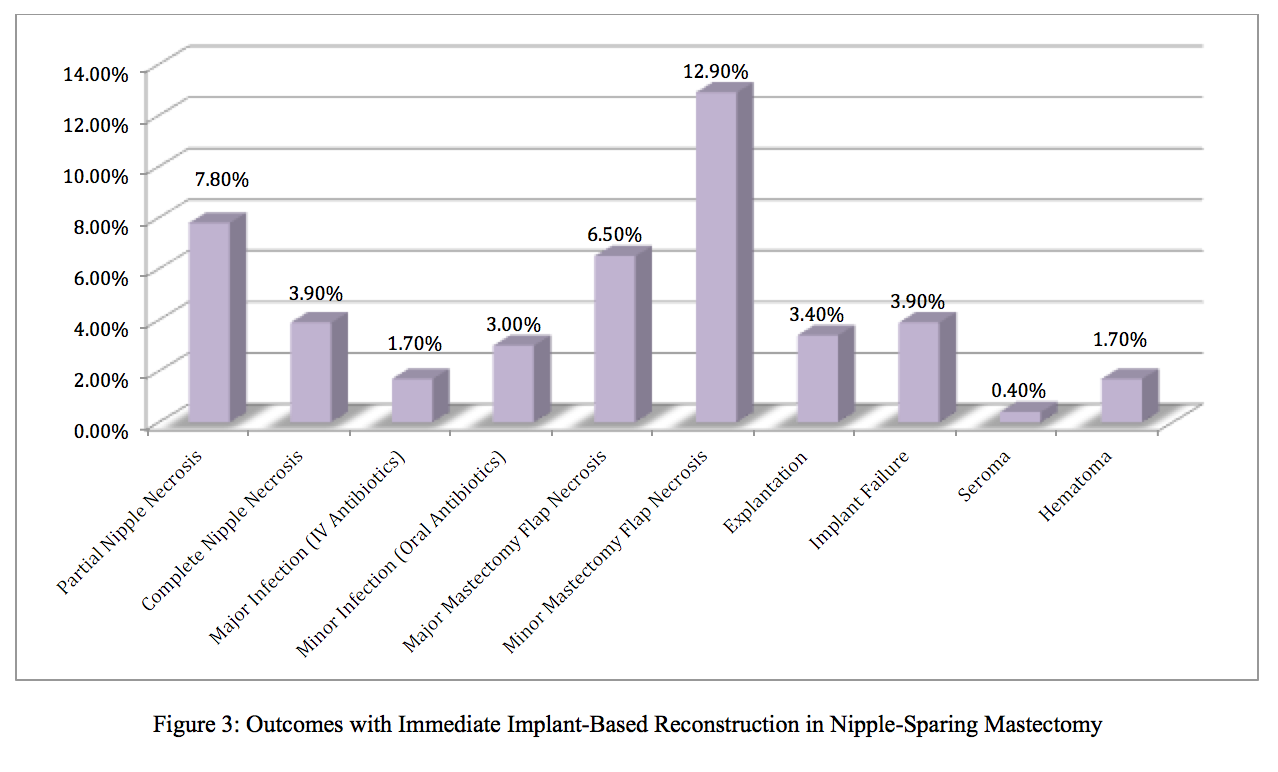
A total of 1028 NSMs were performed; 533 (51.8%) were TE-, 263 (25.6%) autologous-, and 232 (22.6%) immediate implant-based reconstructions.
Compared to autologous reconstructions, TE-based reconstructions had significantly greater smoking history (p=0.0061), lateral radial mastectomy incisions (p<0.0001), as well as post-operative radiation (p=0.0139) and chemotherapy (p=0.0041). Autologous reconstructions had significantly greater body-mass index (p<0.0001), pre-operative radiation (p=0.042), and vertical radial mastectomy incisions (p<0.0001). TE-based reconstructions had significantly more minor cellulitis (p=0.0002) and less complete nipple necrosis (p=0.0126) and major mastectomy flap necrosis (p<0.0001) compared to autologous-based reconstructions.
Compared to immediate implant-based reconstructions, TE-based reconstructions had significantly greater follow-up time (p<0.0001) and lateral radial mastectomy incisions (p<0.0001). Immediate implant-based reconstructions had significantly greater smoking history (p=0.0005). TE-based reconstructions had significantly less initial implant fill/size and less
acellular dermal matrix utilization (p<0.0001, each). TE-based reconstructions had significantly more minor cellulitis (p=0.0006) and less complete nipple necrosis (p=0.0005) as well as major (p<0.0001) and minor (p=0.0028) mastectomy flap necrosis (p=0.0059) compared to immediate implant-based reconstruction.
Compared to immediate implant-based reconstructions, autologous reconstructions had significantly greater follow-up time (p<0.0001), body-mass index (p<0.0001), pre-operative radiation (p=0.0108) and chemotherapy (p=0.0383) and vertical radial mastectomy incisions (p<0.0001). Immediate implant-based reconstructions had significantly greater smoking history (p<0.0001), diabetes mellitus (p=0.030), inframammary fold mastectomy incisions (p<0.0001) and post-operative chemotherapy (p=0.0011) Immediate implant-based reconstructions had significantly more minor cellulitis (p=0.0051), minor mastectomy flap necrosis (p=0.0425), and partial nipple necrosis (p=0.0437) compared to autologous-based reconstructions.
In a logistic regression analysis, age (p=0.030), BMI (p=0.00), as well as prior incision (p=0.028) and Wise pattern (p=0.001) mastectomy incisions were identified as predictors for complications. TE- (p=0.309), immediate implant- (p=0.183), and autologous-based (p=0.692) reconstructions were not significantly predictive of complications.
Conclusions:
Tissue expander, immediate implant, and autologous breast reconstruction techniques may all be safely offered with NSM. However, reconstructive complications appear to be greater with immediate implant- and autologous-based techniques compared to TE-based reconstruction.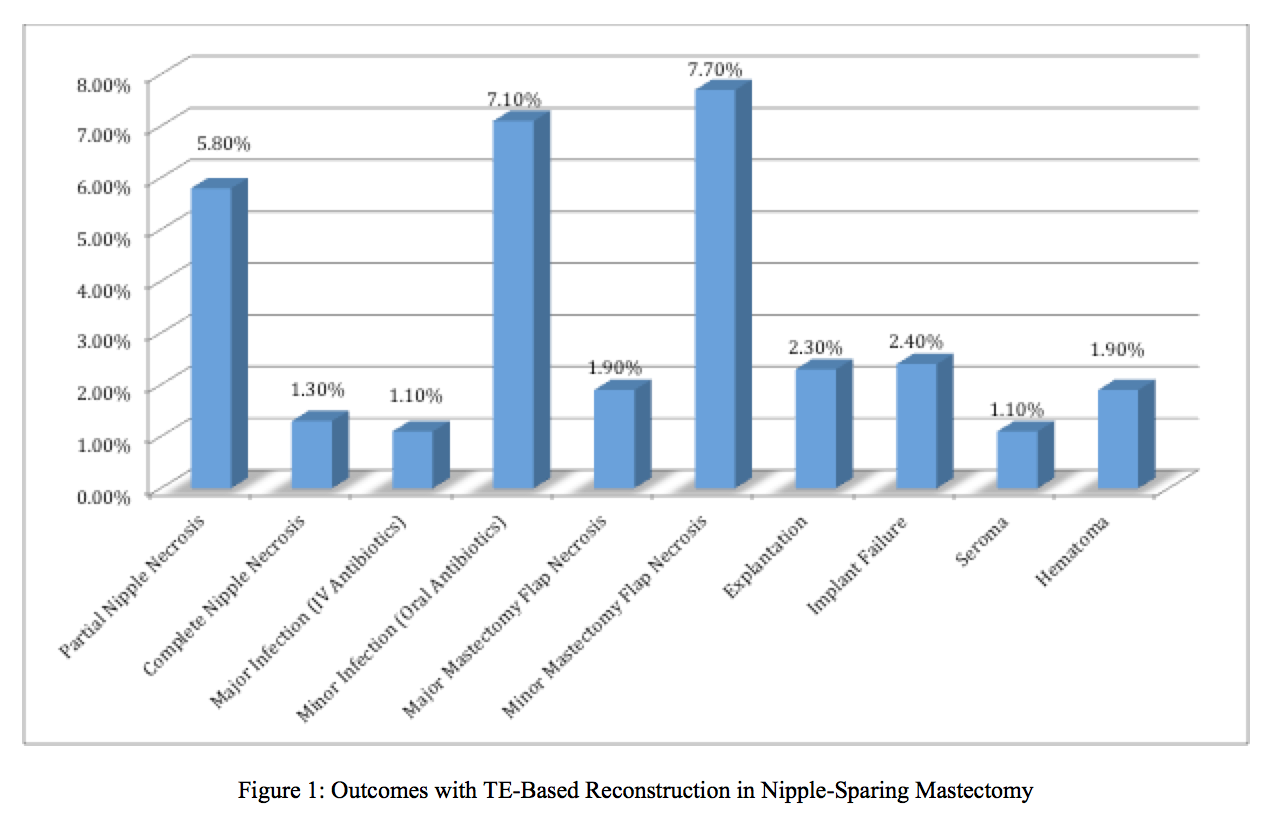
Back to 2017 Program




