A Systematic Review of Sensory Outcomes of Digital Nerve Gap Reconstruction with Autograft, Allograft, and Conduit
Jaclyn T. Mauch, BA, Alison Bae, MD, Valeriy Shubinets, MD, Irfan A. Rhemtulla, MD, MS, Ines C. Lin, MD.
University of Pennsylvania, Philadelphia, PA, USA.
Background: Published literature of digital nerve repairs have not directly compared nerve autograft, nerve conduit, and nerve allograft. This study aims to perform a systematic review to compare the sensory outcomes and complications of nerve autografts, nerve allografts, and nerve conduits relative to primary repair (PR) to elucidate the optimal technique for digital nerve gap reconstruction.
Methods: A review of literature related to digital nerve gap repairs was conducted using PubMed/MEDLINE. Included papers were human clinical studies on digital nerve injuries repaired with nerve autograft, allograft, conduit, or PR. Patient characteristics, injury details, and complications were collected. Greater than 6-month outcomes were measured by static 2-point discrimination (S2PD), the British Medical Research Council Scale (BMRC), or Semmes-Weinstein (SW).
Results: The literature review returned 4 autograft, 4 allograft, 5 conduit, and 7 PR publications, reporting 70 autograft, 66 allograft, 101 conduit, and 569 primary repairs. Allografts had the lowest percentage of sharp injuries (29%), followed by autografts (41%), conduits (65%), and PR (73%). Autografts had a longer mean gap length (22 mm) than allografts (13 mm) or conduits (12 mm). When comparing S2PD results, allografts had the highest percentage of patients (100%) with S2PD <15mm, followed by autografts (88%), conduits (72%), and PR (63%) (Table 1). In BMRC results, autografts (88%) and allografts (86%) were similar for patients with at least S3+ sensibility, while nerve conduit (77%) and PR (39%) studies reported fewer patients in that group. For SW outcomes, patients in the autograft group had the best return of sensation with 93% normal sensation or diminished light touch, compared to allografts (71%) or PR (70%). Nerve conduits had only 36% of patients with normal sensation or diminished light touch. 29% of nerve conduit patients had either loss of protective sensation or anesthetic outcomes, whereas these categories were 0% to 11% in the other groups. Nerve conduits had the highest percentage of complications (11.2%), followed by autograft (5.7%), allograft (3.0%), and PR (0.4%).
Conclusions: The results suggest that autografts and allografts have similar rates of normal or near normal sensation by 2PD, BRMC, and SW. Nerve conduit studies reported a higher rate of incomplete recovery of sensation and complications, suggesting they may be best reserved for shorter gaps. 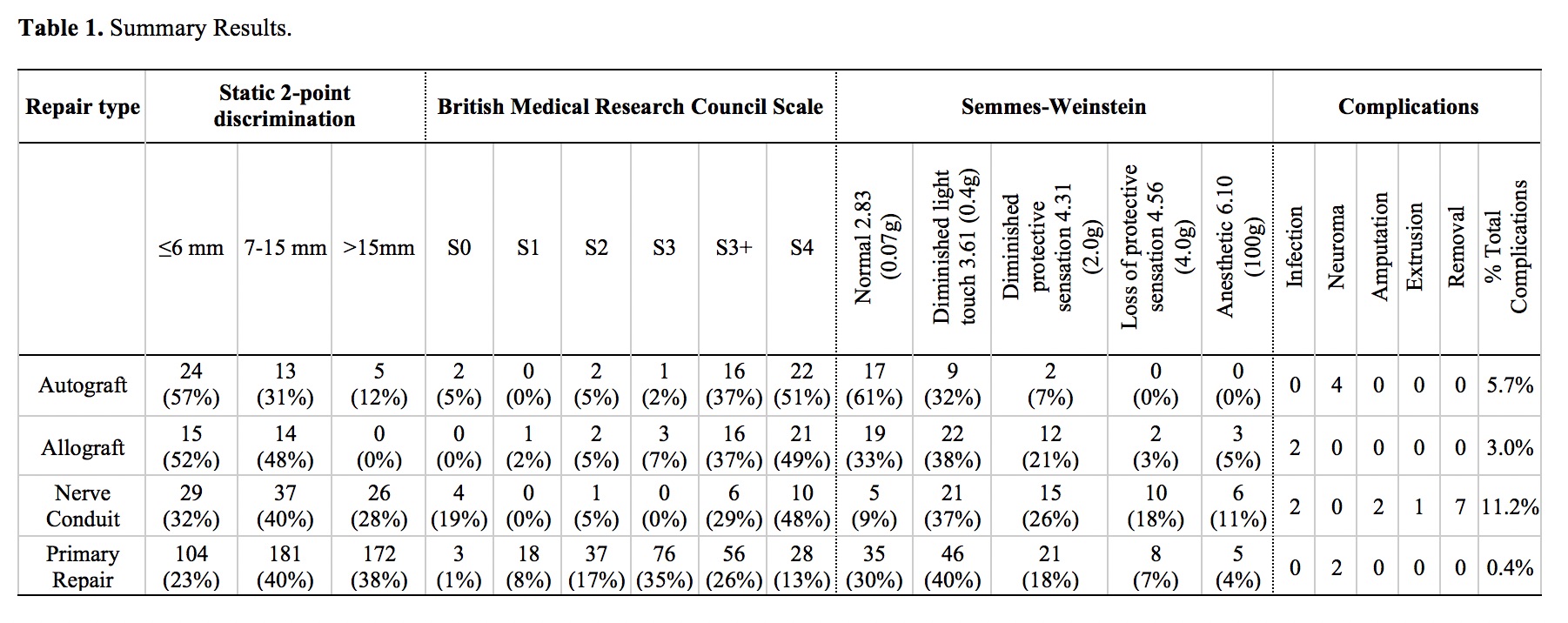
Back to 2018 Abstracts




