Impact of Hospital Volume and Insurance Status on Major Pulmonary Complications after Head and Neck Reconstruction
Leila Musavi, Samuel Sarmiento, MD MBA, Justin Sacks, MD MBA, Oluseyi Aliu, MD.
Johns Hopkins School of Medicine, Baltimore, MD, USA.
BACKGROUND: Head and neck cancer (HNCA) reconstruction is increasingly centralized at high-volume hospitals. However, a significant patient population receives surgical care at low-volume centers, and Medicaid patients comprise a disproportionate fraction of this population. Furthermore, Medicaid patients experience higher mortality after a number of high-risk surgeries. Thus, we examined national HNCA reconstruction trends to assess the impact of hospital volume and insurance status on post-operative pulmonary complications, which are a major source of morbidity in HNCA surgery.
METHODS: We performed a cross-sectional analysis of patients who underwent HNCA resection from 2012-2015 using the National Inpatient Sample. The average number of HNCA cases performed per year of surgical activity was stratified by tertiles to classify hospitals as low-, intermediate-, and high-volume. Major pulmonary complications (including pneumonia, pneumothorax, pulmonary embolism, pleural effusion, and acute pulmonary failure) were dependent variables. Independent variables were age, race, sex, insurance status, comorbidities, prior radiation, reconstruction status, hospital teaching status, and hospital volume
RESULTS: From 2012-2015, 59,975 patients underwent ablative procedures for HNCA; 14,580 (24.3%) received flap or pedicle reconstruction. Hospital volume tertiles were <15,15-65, and >65 cases/year. The majority of patients were white, male, with Medicare or commercial insurance. Mean age was 62 years. Pulmonary complication rate was 10.2% in low-volume and 8.01% in high-volume hospitals. On multivariate analysis, higher hospital volume was associated with lower odds of pulmonary complications (OR 0.52, p<0.001). Pneumonia, pneumothorax, and acute pulmonary failure all had lower odds of occurrence at high-volume compared to low-volume hospitals. Regarding insurance status, Medicaid patients had higher odds of pulmonary complications compared to private payers (OR 1.31, p=0.018). When stratified by hospital volume, Medicaid patients had higher rates of pulmonary complications at both low- and high-volume hospitals. On multivariate analysis, Medicaid status was a significant predictor of complications at high-volume hospitals (OR 1.83, p=0.030) but did not reach statistical significance at low-volume centers (1.37, p=0.361) (Table 1).
CONCLUSIONS: Low surgical volume and Medicaid status are associated with higher odds of post-operative pulmonary complications. Within high-volume hospitals, Medicaid patients have higher odds of complications compared to private payers; at low-volume centers, this association is not statistically significant. These results suggest that insurance status impacts HNCA surgical outcomes and that this relationship may manifest to different extents in low- vs. high-volume hospitals. Further investigation is required to elucidate the relationship between insurance status, hospital volume, and reconstructive outcomes, which will help inform policies to mitigate these disparities. 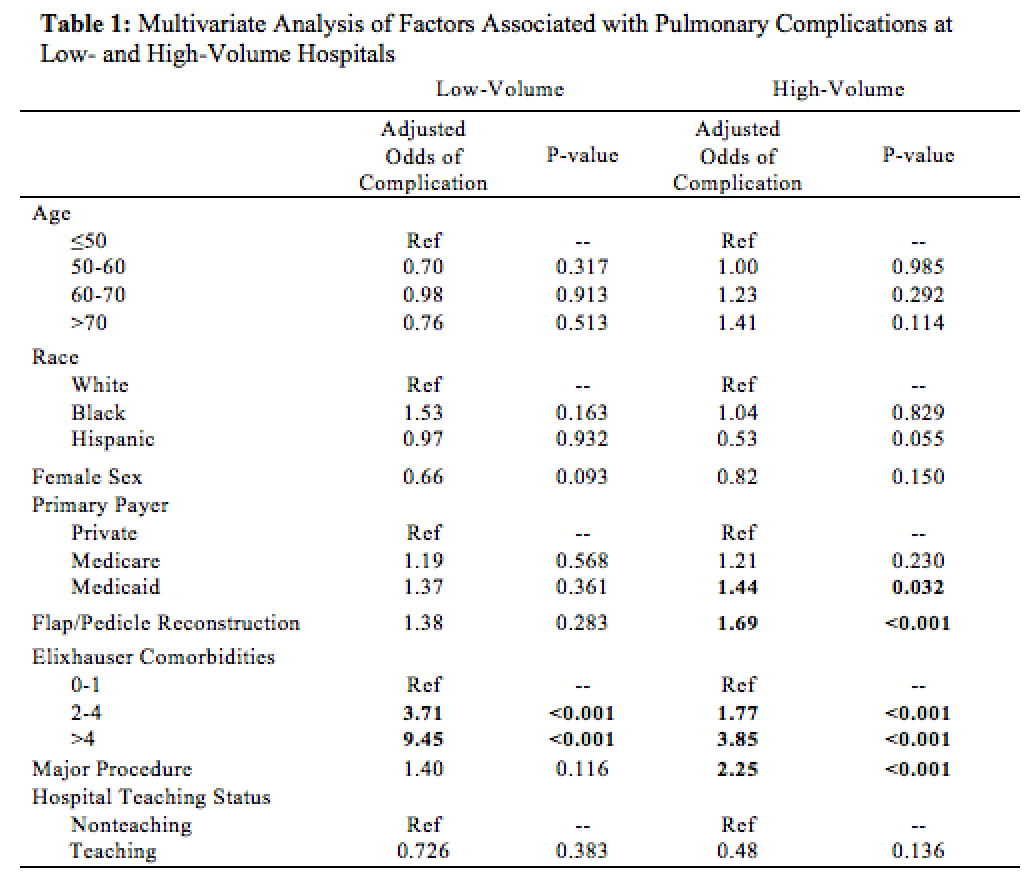
Back to 2018 Abstracts




