Infection After Open Cranial Vault Reconstruction for Craniosynostosis: Institutional Analysis and Systematic Review
Leila Musavi, BA, Joseph Lopez, MD MBA, Regina Cho, BS, Nick Seigel, BS, Amir Dorafshar, MBChB, Jordan Steinberg, MD PhD.
Johns Hopkins School of Medicine, Baltimore, MD, USA.
BACKGROUND: Surgical site infection, while relatively uncommon after open cranial vault reconstruction (CVR), has received little attention in the literature to date. Reported infection rates range from 1.2-8%. Currently, wide variation exists in perioperative management among craniofacial surgeons, but there has been no study thus far consolidating the literature on the topic. Here, we report our institutionís experience with perioperative management of infection after CVR for craniosynostosis and present a systematic review of infectious rates and management practices across the literature.
METHODS: We performed a retrospective chart review of all pediatric patients with syndromic and non-syndromic craniosynostosis who underwent CVR between 1990-2015 at the Johns Hopkins Hospital. Demographic information, comorbidities, suture involvement, surgical procedure, and postoperative course including the occurrence of complications were collected for each patient. For the systematic review, we performed an electronic search of Medline, Embase, Cochrane Index Database, Web of Science, and Scopus. Inclusion criteria were studies in the English language published after 1980 that reported surgical site infections (SSI) after CVR for pediatric craniosynostosis. Exclusion criteria were (1) patients older than 18 years of age, (2) patients with non-synostotic craniofacial abnormalities, (3) endoscopic or distraction procedures, (4) no mention of infection rate.
RESULTS: Between 1990-2015, 548 unique patients underwent CVR for the correction of craniosynostosis at the Johns Hopkins Hospital. There were 163 re-operative procedures. Six patients out of 548 primary reconstructions (1.1%) and 10 out of the 163 reoperations (6.1%) developed SSIs; this difference was statistically significant (p<0.001). On multivariate analysis, syndromic status was associated with SSI (OR 12.0, p=0.007) (Table 1). Our literature search returned 1,641 citations; 30 met inclusion criteria. Across all studies, pooled analysis yielded an overall SSI rate of 1.82% (95% CI 1.24-2.40%). The most common type of SSI was soft-tissue infection, which accounted for 74% of SSIs, followed by hardware infection at 13%. The most common infectious organisms were candida species and P. aeruginosa. The most common antibiotic prophylaxis protocol was a first-generation cephalosporin for 24-72 hours post-operatively.
CONCLUSIONS: At our institution, infection rate was significantly higher in craniosynostosis patients who underwent secondary reconstruction. Syndromic status is an independent predictor of SSI on multivariate analysis. The systematic review of the literature reveals diverse management practices. Our study highlights the role of patient risk factors and clinical practices in the development of infection after intracranial reconstruction, and future work should focus on areas of improvement to optimize patient outcome. 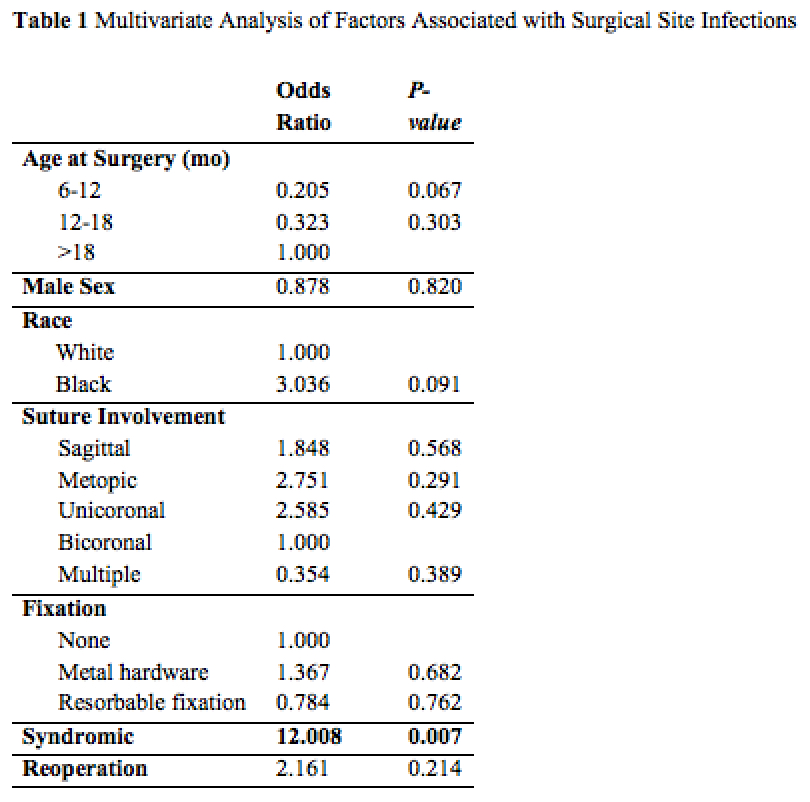
Back to 2018 Posters




