Free dermal fat autografts for complex craniofacial wounds: a three-decade, retrospective cohort study
Craig R. Dufresne, MD, Mikaela I. Poling, BA.
Craig R Dufresne, MD, PC, Fairfax, VA, USA.
BACKGROUND: Complex craniofacial wounds (CCW) are those refractory to initial treatment and may involve chronic infection, exposed hardware, irradiated tissue, and soft tissue volume loss. The reconstruction using free microvascular flaps involves considerable morbidity, is resource intensive, and cannot be used for immediate reconstruction in CCW. While free dermal fat autografting (DFA) is used extensively in many applications, its use treating CCW remains an unexplored but potentially attractive possibility. Aims are to (1) determine if free DFAs are an appropriate adjunct to eradicate infection or provide coverage for exposed hardware in CCW and (2) evaluate if free DFAs are a stable volume and contour reconstructive option for CCW.
METHODS: Data extracted from office charts of a retrospective cohort comprising 33 consecutive patients (13 male; 20 female and aged 2- and 79-years), who underwent free DFA between 1985 and 2018 for CCW by a single plastic surgeon, were analyzed. Post-operative follow-up was 1-24 years (M=6.53, SD=7.91).
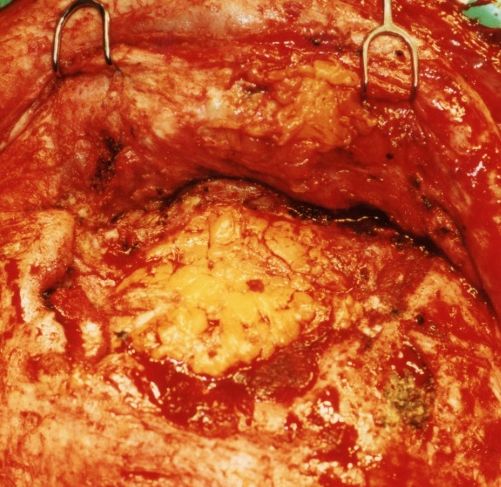
RESULTS: Many patients had several concomitant wound complications. Most patients presented with a history of fracture caused by trauma. Primary pre-operative wound complications (Table 1) were dominated by infection (N 19), of which over 73% (N 14) were associated with non-autologous material. Seventeen had resolution of their pre-operative infection. Of the total (N 33), 78.79% were had stable grafts at follow-up [X2(3)=51.24, p<0.001], with only 3 experiencing observable atrophy and 1 graft necrosis. In 4 patients, free DFAs were palpated during subsequent operative settings and found to be grossly intact, soft, and bleeding (Fig 1). Most of the cohort was complication free [X2(1)=8.76, p=0.003], with 75.76% experiencing no problems involving the graft. Twenty-eight (84.85%) of 33 patients had therapeutic success with free DFA [X2(1)=16.03, p<0.001]. Mechanism of injury (β=0.34, p=0.037) and pre-operative wound status (β=0.42, p=0.016) predicted therapeutic success [R2=0.96, F(11,6)=12.6, p=0.003]. While 5 (15.15%) did not have therapeutic success, no additional problems arose related to graft.
CONCLUSIONS: Free DFA appears to be beneficial for treatment of CCW, showing low morbidity, graft survival and volume stability, effectiveness eradicating infection, and importantly, allowing immediate reconstruction. If substantiated in our on-going cross-sectional and prospective studies, these findings could herald a paradigm shift in research and therapy for CCW away from non-autologous products and free microvascular flaps.
| Primary pre-operative wound complications | Number | Percent |
| Infection | 19 | 57.58 |
| Exposed hardware | 2 | 6.06 |
| Excessive scar tissue | 3 | 9.09 |
| Irradiated tissue | 1 | 3.03 |
| Soft tissue hypoplasia or defect | 8 | 24.24 |
Back to 2019 Abstracts
