The Association of Zygomaticomaxillary Complex Fractures with Naso-Orbito-Ethmoid Fractures in Pediatric Populations
Pooja S. Yesantharao, MS1, Joseph Lopez, MD, MBA1, Amy Chang, MPH2, Jacqueline Hicks, MS, PhD2, Gianni Thomas, BA1, Maria Reategui, BA1, Paul N. Manson, MD1, Amir Dorafshar, MBChB3, Richard J. Redett, III, MD1.
1Johns Hopkins School of Medicine, Baltimore, MD, USA, 2Boston University School of Public Health, Boston, MA, USA, 3Rush Medical College, Chicago, IL, USA.
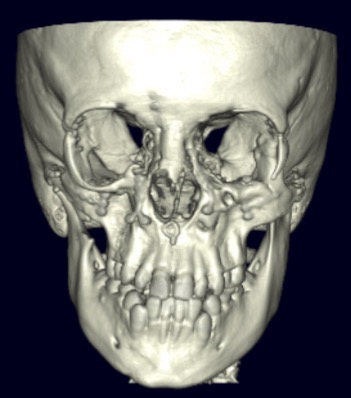
BACKGROUND: Naso-orbito-ethmoidal (NOE) fractures associated with ipsilateral ZMC fractures are more challenging injuries than ZMC fractures alone. However, there is a paucity of information on this complex fracture pattern in pediatric patients. This study investigated the etiology, treatment, and outcomes of combined ZMC-NOE fractures versus isolated ZMC fractures in children.
METHODS: This is a 20-year retrospective cohort study of pediatric patients who presented to a single institution with ZMC fractures. Baseline patient demographics and clinical information, as well as concomitant injuries, treatment/operative management, and postoperative complications/deformities were recorded and compared between patients with combined ZMC-NOE fractures and patients with isolated ZMC fractures.
RESULTS: Forty-eight patients had ZMC fractures in our 20-year study period, of whom forty-five had adequate documentation and follow up. Seventeen of these patients had ipsilateral NOE injuries associated with their ZMC fractures. Both patient groups (isolated ZMC fractures and combined ZMC-NOE fractures) were similar in terms of demographics. However, patients with combined ZMC-NOE fractures had longer median hospital lengths of stay. Furthermore, a greater proportion of patients with combined ZMC-NOE fractures required extensive surgical approaches with coronal incision when compared to patients with ZMC fractures alone (57.1% vs. 11.8%, p=0.007). Approximately 88.2% of patients with combined ZMC-NOE fractures suffered complications versus 32.1% of patients with isolated ZMC fractures (adjusted odds ratio 58.2, p = 0.001; Table 1). Patients with combined ZMC-NOE fractures also had greater incidence of postoperative facial deformity than those with ZMC fractures alone (adjusted odds ratio 6.72, p = 0.032). Enophthalmos (41.2%) and midface growth restriction (35.3%) were the two most common postoperative deformities in patients with combined ZMC-NOE fractures - in fact, midface retrusion was seen exclusively in patients with this combined fracture pattern.
CONCLUSIONS: This is the largest study of combined ZMC-NOE fractures in pediatric patients. Our results demonstrate that high-impact trauma can cause NOE fractures in association with ZMC fractures relatively commonly in children. This injury pattern was found to cause significantly greater postoperative rates of complication and deformity than isolated ZMC fractures, possibly due in part to inadequate reduction in the context of a more complex fracture. Thus, pediatric patients presenting with this fracture pattern require greater attention at the time of operative repair to ensure adequate bony reduction. Furthermore, these patients require more extensive clinical monitoring given a greater risk for long-term morbidity.
Table 1: Complications and Deformities for Isolated ZMC Fracture versus Combined ZMC+NOE Fracture Patients (n=45)
| ZMC (n=28) | ZMC+NOE (n=17) | |
| Complications – n (%) | 9 (32.1) | 15 (88.2) |
| Major Strabismus/Diplopia Cellulitis Osteomyelitis Hardware Infection Hardware Extrusion | 3 (10.7) 1 (3.6) 0 (0.0) 1 (3.6) 1 (3.6) | 6 (35.3) 4 (23.5) 1 (5.9) 1 (5.9) 4 (23.5) |
| Minor Nasolacrimal Duct Obstruction Sinusitis CSF Rhinorrhea Dacryocystitis Keloid Formation Hypertrophic Scar Formation Scar Contracture Hematoma Anosmia Septal Deviation Ectropion | 2 (7.1) 1 (3.6) 0 (0.0) 0 (0.0) 0 (0.0) 3 (10.7) 2 (7.1) 3 (10.7) 0 (0.0) 0 (0.0) 3 (10.7) | 5 (29.4) 4 (23.5) 2 (11.8) 2 (11.8) 1 (5.9) 8 (47.1) 11 (64.7) 1 (5.9) 1 (5.9) 6 (35.3) 5 (29.4) |
| Deformity Enophthalmos Orbital Dystopia Midface Retrusion Midface Asymmetry Telecanthus Fracture Nonunion Dental Malocclusion | 3 (10.7) 2 (7.1) 0 (0.0) 3 (10.7) 1 (3.6) 0 (0.0) 1 (3.6) | 7 (41.2) 5 (29.4) 6 (35.3) 2 (11.8) 3 (17.6) 1 (5.9) 4 (23.5) |
Back to 2019 Abstracts
