The Effect of Topical Tacrolimus on Pedicled Flap Survival: The Secret Is in the Sauce
Y-vu R. Van1, Gal Wald2, Connie Lu2, Arash Samadi2, David Otterburn2.
1New York Presbyterian, NY, NY, USA, 2Weill Cornell Medical College, NY, NY, USA.
BACKGROUND: Skin necrosis is a known postoperative complication of mastectomies. The pathophysiology of tissue necrosis involves lymphatic congestion, followed by venous congestion and ultimately arterial insufficiency. Recent mouse model studies have shown topical tacrolimus to increase growth of lymphatic collateral vessels and decrease lymphedema, potentially obviating the cycle of necrosis and increasing skin survival. The purpose of this study is to investigate the effect of topical tacrolimus on skin flap necrosis in a rat model. METHODS: A 3x10cm cranially based dorsal skin flap was raised and re-inset on twenty-two Sprague Dawley rats. They were then randomized to either the control (topical petroleum jelly) or the treatment (topical 0.1% tacrolimus) arm. 0.2 grams of either ointment was spread over the flap and then covered with an occlusive dressing. Dressings were changed daily with reapplication of both the topical ointment and the occlusive dressing. The rats were sacrificed 7 days post-op; areas of viable tissue, reversible ischemia and full thickness necrosis were measured with Fiji software and comparative analysis was performed with GraphPad statistical software. RESULTS: The average area of the dorsal flaps in the control and tacrolimus groups was 22.5 and 23.9 cm2, respectively. In the control cohort, the average viable area was 42.4%, the average reversible ischemia area was 43.6%, and the average necrotic area was 13.9%. In the tacrolimus cohort, the average viable area was 31.5%, the average reversible ischemia area was 59.3%, and the average necrotic area was 9.2%. Total necrotic area was significantly lower in rats receiving topical tacrolimus as compared to controls (p=0.015). Furthermore, the ratios of necrotic to reversible ischemia and necrotic to viable tissue were significantly lower in the tacrolimus group as compared to controls (p=0.003, p=0.015). Of note, there was one incidence of wound dehiscence secondary to rodent self-removal of Tegaderm and suture that required re-operation and re-inset. There were no other complications. CONCLUSIONS: Topical tacrolimus was associated with significantly less full thickness necrosis as compared to topical petroleum jelly in this model. Future animal studies investigating dosages, differences in pre and post-operative application, and histological examination will further delineate the use of tacrolimus in flap healing, survival and eventual clinical use. 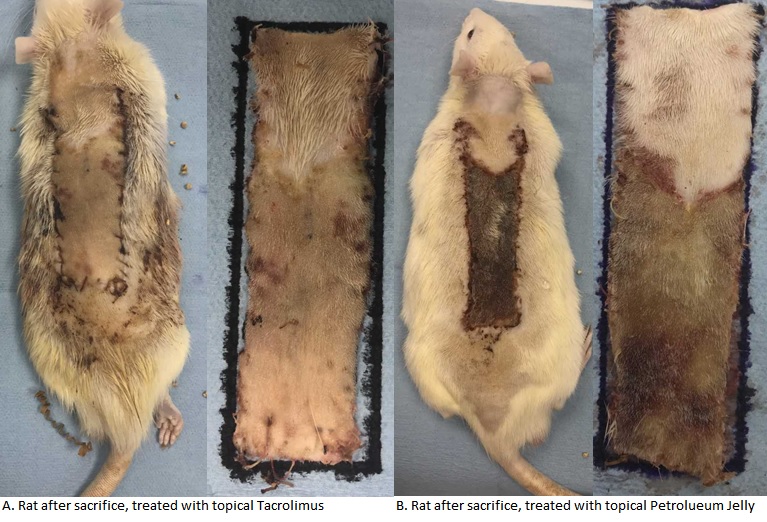
Back to 2019 Abstracts
