The Development of Novel Low-Cost, High impact Models: Can Simulation Survive in Plastic Surgery Education?
Joanna H. Ng-Glazier, MD, Jeffrey A. Gusenoff, MD.
University of Pittsburgh, Pittsburgh, PA, USA.
BACKGROUND: Studies suggest that integration of a formal simulation is beneficial to surgical trainees, but its role has not been well defined in plastic surgery.
METHODS: Residents at a large ACGME-accredited plastic surgery program identified several topics of technical deficiency in their current educational structure. A multi-session curriculum spanning 6 months (July 2018-January 2019) was developed to address these topics, each supplemented by electronically accessible material. Using low cost materials, four models were created to target skills in breast surgery marking, ultrasound guided aspiration and injection, safe buttock augmentation, and pinning/drilling across hand and joint fractures. Improvement in knowledge, comfort of technical skill after each session, quality of models, supplemental materials, and overall resident satisfaction were measured immediately after each session and compared via paired t-test, α=0.05.RESULTS: 24 residents (100% participation) identified clinical deficiencies in the following: preoperative breast markings, use of ultrasound for bedside procedures, comfort with gluteal fat injection, and drilling and pinning fractures. Utilizing a scale of 1-10, average post-simulation knowledge and skill comfort doubled for all sessions, including breast markings (4.32 à7.00, p<0.01), ultrasound-guided aspiration of abscess, seroma, upper extremity nerve blocks, gluteal fat injection (3.65 à7.25, p<0.01), and drilling/pinning hand and joint fractures (3.15 à6.56, p<0.01). Satisfaction ratings were 8.64, 9.13, and 9.25, respectively. Stratification by training year indicated greater impact in junior residents (R1-3) for drilling/pinning compared with senior residents (R4-6), but no difference in breast markings or ultrasound procedures. Stratification between integrated and independent/traditional pathway residents indicated higher impact for traditional residents in all sessions except for ultrasound. 100% of residents desired continued skill simulation with the current models. CONCLUSIONS: Repetitive skill simulation using reusable low-cost, high impact models has the potential to supplement our current plastic surgery resident education. Long term validation, skill retention, and well as Identification of targeted skills for each training level is necessary for ongoing assessment. 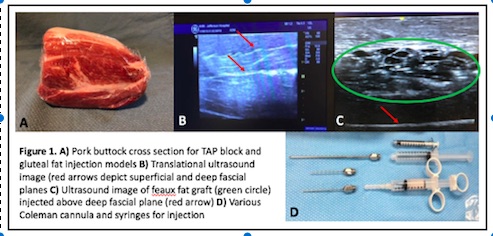
Back to 2019 Abstracts
