A Retrospective Analysis of GERD in the Cleft Palate Population and Implications for Treatment of Failure to Thrive
Ishani D. Premaratne, BA1, Nicholas Brownstone, MD1, Philip Lotfi, MD1, Thomas Imahiyerobo, MD2.
1Weill Cornell Medicine, New York, NY, USA, 2Columbia University Medical Center, New York, NY, USA.
Background: As compared to the general pediatric population, patients with cleft lip and/or palate are burdened by increased rates of failure to thrive (FTT) and feeding difficulties. While insufficient nursing, excessive air intake and incorrect feeding methods have been studied, we believe that a higher rate of gastroesophageal reflux disease (GERD) in cleft patients may be a contributing factor. There is limited data analyzing the effect of GERD on feeding and weight gain. The purpose of this study is to identify the incidence of GERD in the cleft population and to see if appropriate treatment was effective in improving weight gain and decreasing rates of FTT in patients undergoing primary cleft surgery.
Methods: A retrospective review included fifty patients with cleft lip, cleft lip and palate and isolated cleft palate who were treated by a single surgeon from 2015-2019. Collected information included type of cleft deformity, evidence of GERD, visits to other medical specialties, evidence of FTT, and treatment of GERD. The impact of GERD treatment on weight gain in the cleft population was compared to cleft patients without a diagnosis of GERD.
Results: The average age of the cohort was 1.7 years. 48% of patients with cleft lip/and or palate had clinical evidence of GERD requiring treatment. 67% of patients with isolated cleft palate, 41% of patients with cleft lip and palate and 33% of patients with cleft lip were diagnosed with GERD. Of these patients, 66% were treated with behavioral adjustment (upright positioning after feeds, change in bottle or nipple system) and 33% received pharmacologic treatment with either ranitidine or lansoprazole (Figure 1). In patients with GERD, 16% required a feeding tube vs. 4% in non-GERD patients. The rate of FTT in the patients with GERD diagnosis was 33%, which represented 89% of the incidence of FTT in the cohort. A chi-square analysis showed a significant association between the diagnosis of GERD and FTT (X2 =7.35, p < 0.05). A difference-in-differences showed a significant increase in weight from time of initiation of GERD treatment to time of surgery (R2 =0.428, P<0.05).
Conclusions: This study demonstrates that the diagnosis of GERD is significantly higher in the cleft population than previously reported, with a concomitant association between diagnosis of GERD in cleft patients and FTT. Patients showed significant weight gain once GERD treatment was initiated, providing evidence for consideration of GERD treatment in all cleft patients who present with FTT. 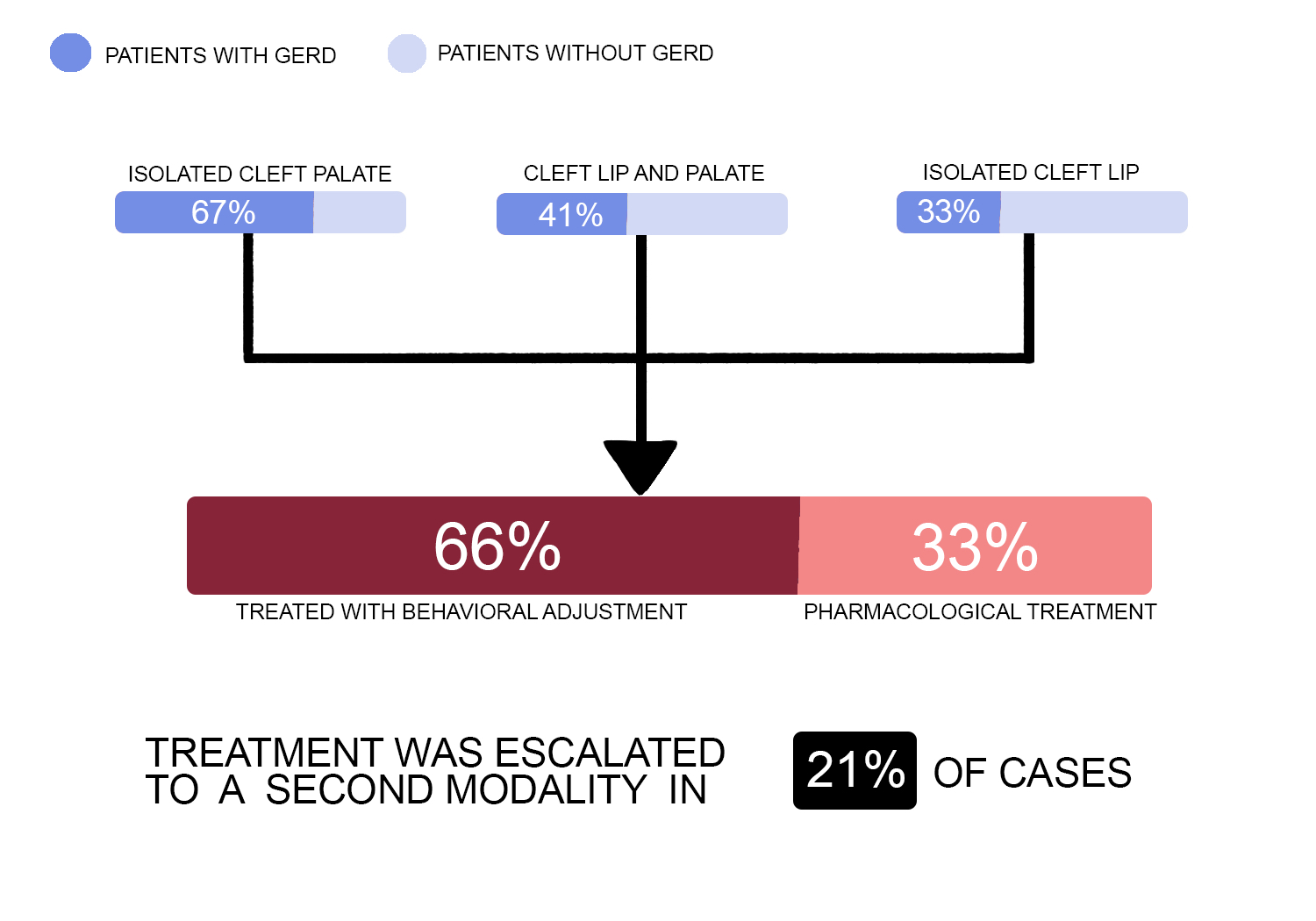
Back to 2019 Abstracts
