Impact of Comorbidities on Institution-specific Normative Data for the BREAST-Q Reconstruction Module
Kevin M. Klifto, PharmD, Pathik Aravind, MBBS, Rachael M. Payne, MD, Wen Shen, MD, MPH, Gedge D. Rosson, MD, Michele A. Manahan, MD, MBA, Carisa M. Cooney, MPH.
The Johns Hopkins University School of Medicine, Baltimore, MD, USA.
BACKGROUND: The BREAST-Q has been used extensively to assess patient-reported breast surgery outcomes; however, breast satisfaction in a general female population is relatively unknown and prior research has not evaluated the impacts of different comorbidities on scores. We sought to assess the impact of participant-related comorbidities on breast satisfaction and quality-of-life (QOL) in women without breast cancer or a history of breast surgery to establish normative BREAST-Q scores accounting for comorbidities.
METHODS: This is a cross-sectional, single-center study of patient-reported outcomes using the BREAST-Q. A preoperative BREAST-Q reconstruction module and demographic form were administered to female participants who presented for routine gynecology appointments. Eligible patients were women with no history of breast cancer or breast surgery and were not pregnant. We assessed participant-related comorbidities to evaluate the impact on BREAST-Q scores using linear multivariate regression analysis and compared differences between participants who did and did not have these comorbidities at the time of BREAST-Q completion. Median BREAST-Q scores were compared using the minimal important difference (MID) greater than 0.5 standard deviations to establish clinical significance.
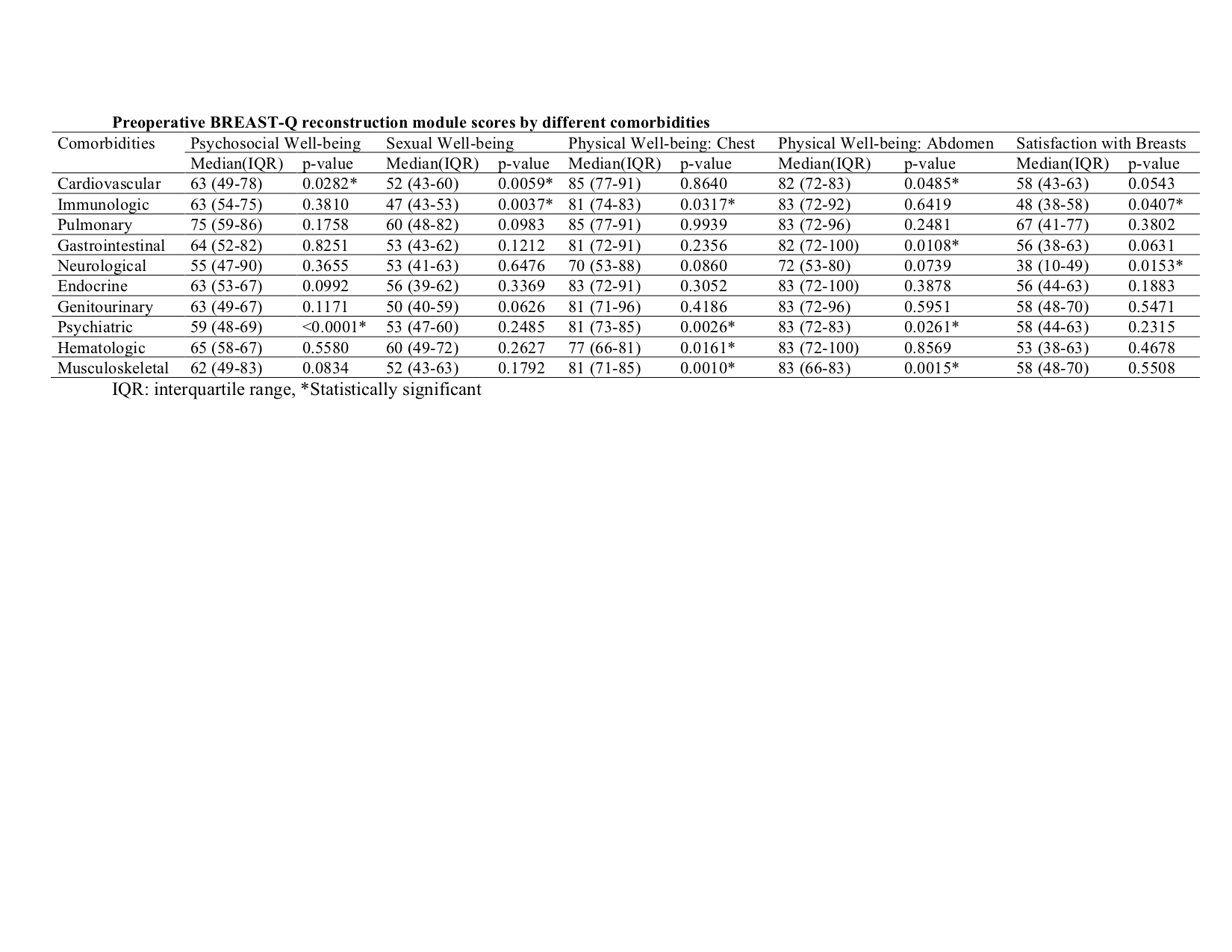
RESULTS: Three hundred female participants were included in the study (n=300). Fifty-six participants had cardiovascular disease, 17 had immunologic disease, 28 had pulmonary disease, 32 had gastrointestinal disease, 4 had neurological disease, 36 had endocrine disease, 16 had genitourinary disease, 52 had psychiatric disease, 7 had hematologic disease, and 42 had musculoskeletal disease. Neurological disease (p=0.026) and gastrointestinal disease (p=0.039) were statistically significantly associated with lower Satisfaction with Breasts scores. Psychiatric disease was associated with significantly lower Psychosocial Well-being scores (p<0.0001). Hematologic disease was associated with significantly lower Physical Well-being: Chest scores (p=0.005). Musculoskeletal disease was associated with significantly lower Physical Well-being: Chest scores (p=0.043) and Physical Well-being: Abdomen scores (p=0.036). After comparing MID, Sexual Well-being scores with immunologic disease, Satisfaction with Breasts scores with neurologic disease, Psychosocial Well-being scores with psychiatric disease, and Physical Well-being: Chest scores with hematologic disease were clinically significantly lower with MID>0.5.
CONCLUSIONS: We found that the presence of neurological, gastrointestinal, psychiatric, hematologic, and musculoskeletal comorbidities were associated with lower BREAST-Q scores. Understanding how comorbidities may influence pre-operative BREAST-Q scores in a non-cancer population could help better establish baseline scores for patient-reported outcomes research in breast reconstruction.
Back to 2019 Posters
