A Novel Treatment Algorithm for Retained Temporary Epicardial Pacing Wires
Gal Wald, BA, Robert Van, MD, David Otterburn, MD.
Weill Cornell Medicine, New York, NY, USA.
BACKGROUND: Temporary epicardial pacing wires (TEPW) are used postoperatively for the identification, diagnosis, and treatment of acute arrhythmias. They are usually removed before discharge but are sometimes clipped and left to retract into the skin. Complications from these retained wires have been documented in numerous case reports and are often referred to plastic surgeons as wound healing complications. We performed a systematic review of these patients to delineate complications and to create a novel treatment algorithm.
METHODS: The authors conducted a PRISMA-guided systematic review of MEDLINE, Embase and Cochrane Library databases and retrieved English-language articles published between 1986 and 2018. Two reviewers critically appraised the studies that met inclusion and exclusion criteria. A treatment algorithm was designed based on the results.
RESULTS: Thirty-one articles met inclusion criteria with a total of 35 patients included. The existing articles represent either level IV or level V evidence. 27 patients (77%) were symptomatic with either skin lesion (33%), fever (22%), dyspnea (22%), abdominal pain (11%), chest pain (7%), cerebrovascular events (7%), cough (4%) and/or pelvic pain (4%). Wires caused infection in 20% of cases, as well as abscess formation (11%), sternobronchial fistulas (9%), heart failure (6%), cardiac arrest (6%), and/or hemopericardium (3%) in others. TEPW wire migration occurred in 26/35 (74%) patients, with invasion into vasculature (38%), visceral organs (27%) and subcutaneous tissue (26%). Of the symptomatic patients, 20/27 patients (74%) had wire migration and of symptomatic patients with migration, 19/20 (95%) patients had their wires removed. Symptomatic patients without wire migration had their wires removed in 4/7 cases (57%). Conversely, of the asymptomatic patients, 6/8 patients (75%) had wire migration and of asymptomatic patients with migration, 4/6 (67%) patients had their wires removed. Most of the patients who underwent wire removal had complete recovery.
CONCLUSIONS: In patients with severe symptoms or evidence of migration, surgical intervention and removal should be strongly considered to prevent potentially deadly complications. We propose an algorithm to minimize these complications based on a literature analysis in accordance with PRISMA guidelines. 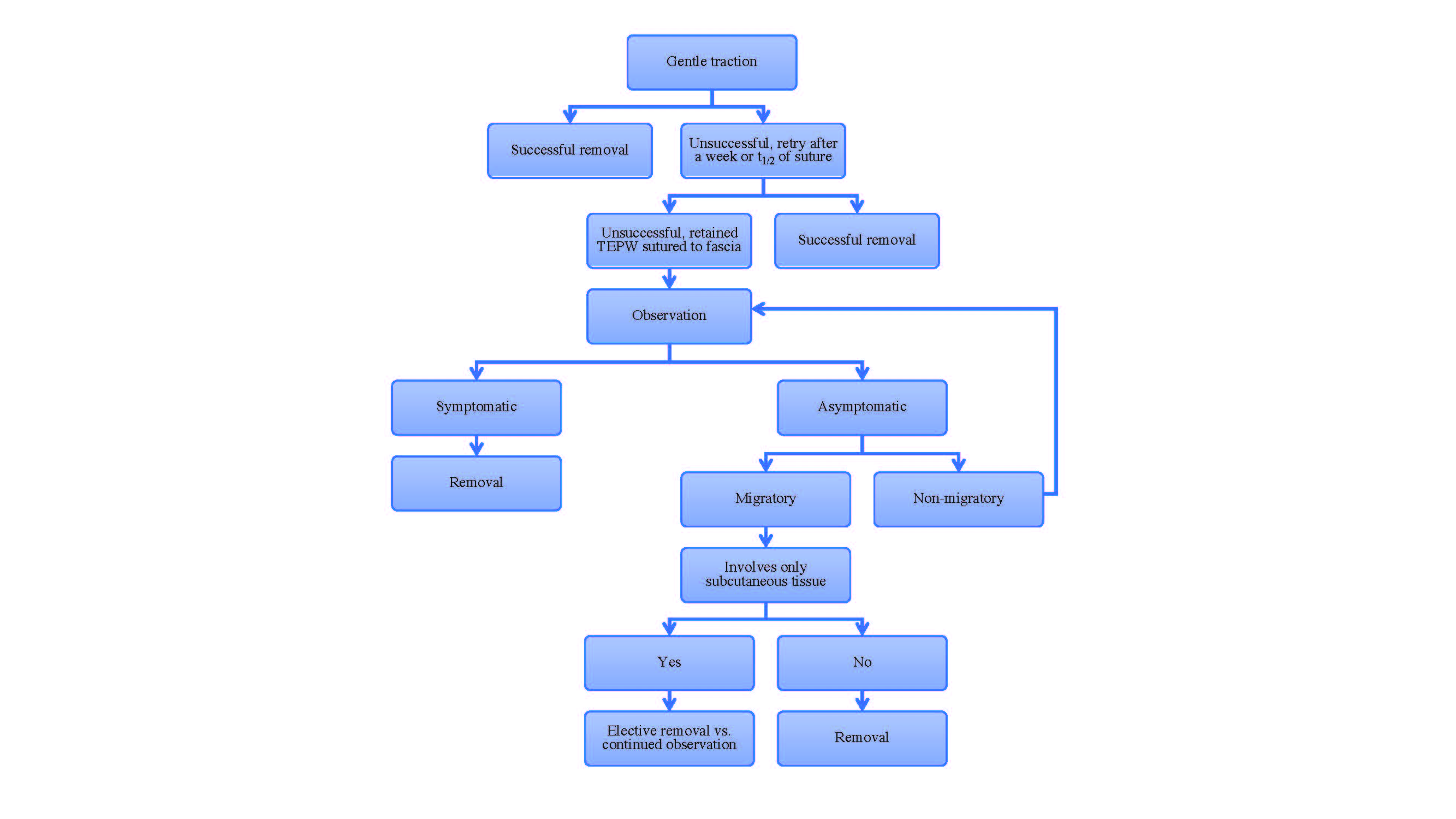
Back to 2019 Posters
