To spare or not to spare the muscle: a single center experience with muscle-sparing thoracotomies
Estifanos D. Tilahun, BS, Takintope Akinbiyi, MD, Suhil Singal, MD, Jordan Swanson, MD.
University of Pennsylvania, Philadelphia, PA, USA.
Purpose/Background:
Lung cancer is the leading cause of cancer death in the world, killing more patients than stomach, breast, and prostate cancers combined1. For those who are surgical candidates, there are numerous approaches, but the gold standard remains the posterolateral thoracotomy (PLT). However, PLT is associated with post-operative issues such as chronic pain, decreases in both shoulder and pulmonary function, and cosmesis2,3,4. These complications are related to the transection of the latissimus dorsi and lower edge of the serratus anterior muscles during the initial exposure. The muscle-sparing thoracotomy (MST) is an alternative to the PLT that has gained some support given its ability to achieve the same exposure while maintaining the integrity of the latissimus and the serratus anterior.
Few studies have compared these two approaches. Most have focused mainly on pain, and shoulder and pulmonary functional outcomes in patients with early stage disease, and not reported on wound complications. Therefore, there is a lack of comparative data in patient populations with more aggressive pulmonary pathology. This study aims to evaluate MST in this patient population and compare with published studies reporting PLT outcomes.
Methods/Technique:
A retrospective review was performed to identify patients who underwent MST at an academic tertiary care center over the last 18 months. Demographics, diagnoses, procedural details, complications and mortality rates were reviewed. These endpoints were then compared to historical studies that reviewed the PLT technique.
Results:
16 patients were identified with an average age of 67.4 years (range 30 to 82 years). 93.75% of cases were neoplastic (13 malignant mesotheliomas, 1 Ewing sarcoma and 1 metastatic thymic squamous cell carcinoma). One patient received treatment for extensive cystic fibrosis disease. There were 13 total complications; 3 dysrhythmias, 5 wound healing complications, 3 pneumonias, 1 empyema, and 1 seroma. There were no associated mortalities.
Conclusion:
In comparison to historic data on PLT outcomes (Table 1), our results demonstrate a favorable complication profile when considering the aggressive nature of the patient disease and resultant radical resections. We also experience only 1 seroma, a complication cited in other reports as a potential consequence of MST5,6, and no mortalities. Future work will involve comparing our MST results to PLT data at our own institution. 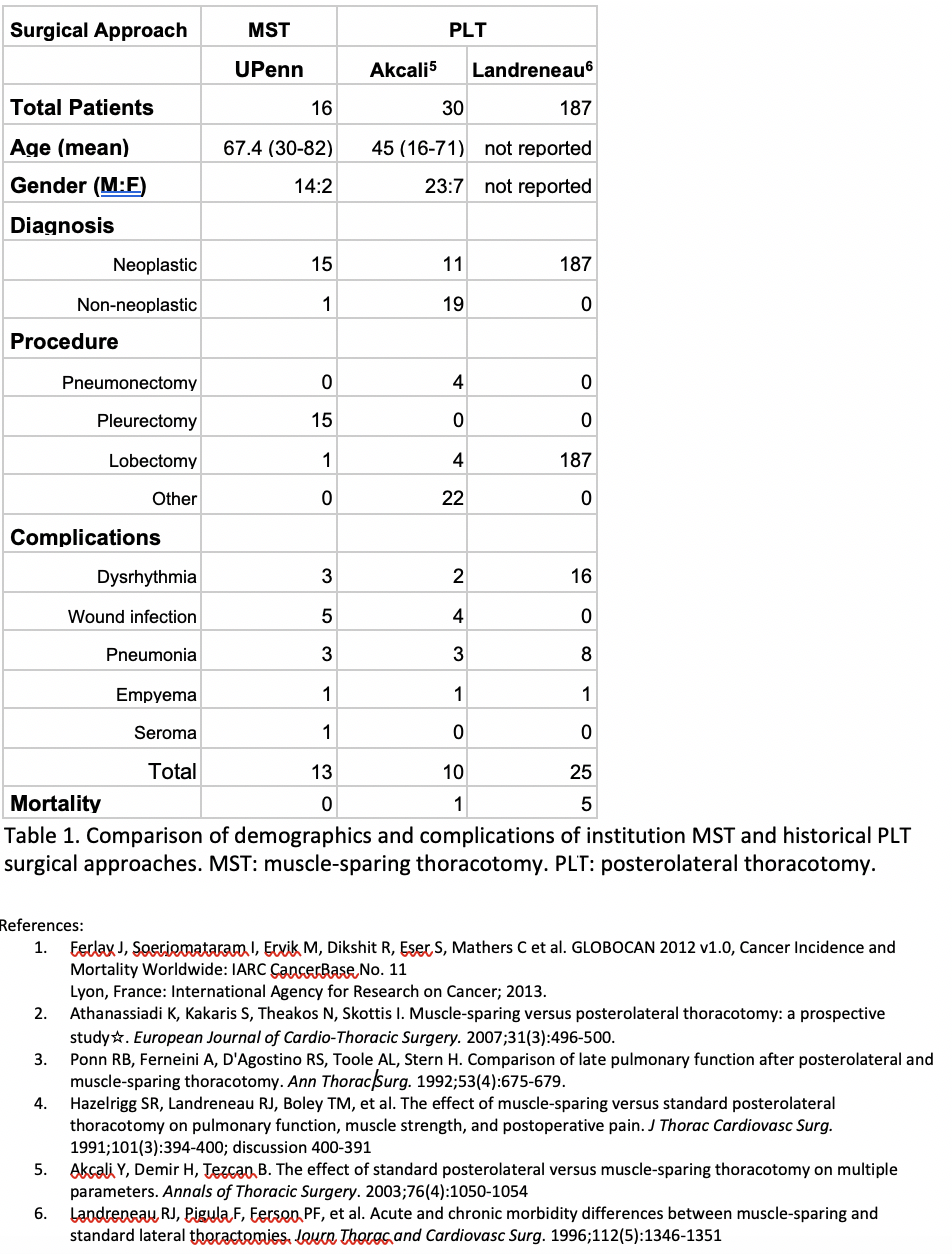
Back to 2019 Posters
