VENT-LOCK: A Plastic and Reconstructive Surgical Innovation Teamís Response to the COVID-19 Pandemic and Ventilator Shortages
Helen Xun, BS1, Christopher Shallal2, Justin Unger, BS2, Runhan Tao, BS, MS2, Alberto Torres, BS2, Michael Vladimirov, BS2, Jenna Frye, BS, MA, MFA3, Mohit Singhala, BS2, Pooja Yesantharao, BS, MS1, Bo Soo Kim, MD1, Justin Sacks, MD, MBA, FACS4, James Guest, PhD2, Sung Hoon Kang, PhD2, Julie Caffrey, DO, MPH1.
1Johns Hopkins School of Medicine, Baltimore, MD, USA, 2Johns Hopkins Whiting School of Engineering, Baltimore, MD, USA, 3Maryland Institute College of Art, Baltimore, MD, USA, 4Washington University in St. Louis, St. Louis, MO, USA.
BACKGROUND: Plastic and reconstructive surgery (PRS) is a collaborative field grounded in generations of surgical and intensive care innovations. In light of the COVID-19 pandemic, our interdisciplinary research team demonstrates the resourcefulness of PRS by developing a safer ventilator splitter, Vent-Lock, to address critical global ventilator shortages. Using one ventilator for multiple patients can increase capacity immediately to address the global shortage of 880,000, but faces challenges and safety concerns including differing patient body habitus, lung compliances and pathologies necessitating individualized ventilator settings, prevention of cross-contamination between patients, and workflow. We address these concerns with the Vent-Lock breathing circuit, featuring the novel flow restrictor, FloRest.
METHODS: We used 3D printing (3DP) to iteratively prototype, test, and optimize Vent-Lock circuit component designs, using biocompatible and sterilizable materials. Designs were created using computer aided design (CAD) and fabricated via stereolithography or fused filament fabrication-based 3DP. Vent-Lock breathing circuits were tested using a ventilator (Nellcor Puritan Bennett, 840 Ventilator System) split for two simulated patients (ASL5000, RespiLung) with differing lung compliances, with continuous intrapulmonary data collection. Vent-Lock was also validated for splitting anesthesia machines (Daytex Ohmeda S/5 Advance) in in vivo swine studies with continuous airway monitoring, arterial blood gases, and histopathology.
RESULTS: We created an 1+n(1) ventilator split circuit with additional safety components (Figure 1a), such as continuous airway monitoring, filters, and one-way valves. It features the Vent-Lock FloRest for tidal volume control on inspiratory loops, and PEEP control on expiratory loops, without affecting pressures or volumes to the other patient (Figure 1b). FloRest costs approximately $3.50 and 4 hours to produce and outperform commercially available valves (Figure 1c). We validated our airtight breathing circuit, and also produced one-way valves integrated into the ventilator splitter and filter drawers with replaceable filters to minimize aerosolization or cross-contamination of viruses. Materials can be safely and quickly sterilized via autoclave or alcohol baths, with no risk of decomposing the device (confirmed by stable particle counts ranging >200 microns). Two swines were stably ventilated for five hours by one anesthesia gas machine, as confirmed by arterial blood gases, continuous airflow monitoring, and final lung histopathology.
CONCLUSIONS: As a field grounded in innovation and ingenuity, plastic and reconstructive surgical innovation teams are well positioned to assist in crisis and pandemic responses. Our team has validated a safer ventilator split circuit to increase ventilator capacity safely to meet urgent ventilator shortages. 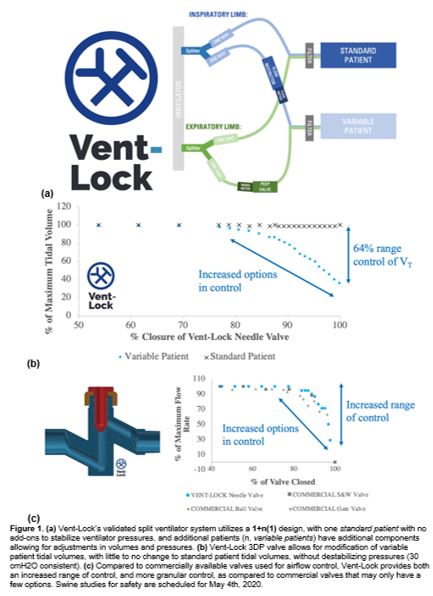
Back to 2020 Abstracts
