Use of Gravity Versus Pulsatile Flow Irrigation Leads to Increased Odds of Infectious Complications in the Lower Extremity Chronic Wound Population
Karina Charipova, BS1, Jenna C. Bekeny, BA2, Elizabeth G. Zolper, BS2, Cameron M. Akbari, MD, MBA3, John S. Steinberg, DPM2, Kenneth L. Fan, MD2, Christopher E. Attinger, MD2, Karen K. Evans, MD2.
1Georgetown University School of Medicine, Washington, DC, USA, 2Department of Plastic Surgery, MedStar Georgetown University Hospital, Washington, DC, USA, 3Department of Vascular Surgery, MedStar Georgetown University Hospital, Washington, DC, USA.
BACKGROUND: Wound irrigation for infection eradication is essential to successful reconstruction. High-pressure irrigation with pulse lavage has similar outcomes to low-pressure irrigation in the acute traumatic population but has not been thoroughly analyzed in comorbid chronic wound patients.1 We investigated outcomes following the change from pulsatile flow to gravity flow irrigation at our tertiary wound center.
METHODS: A single-center retrospective review was performed on patients who underwent surgical debridement of a lower extremity wound from 2017 to 2019 and had documented follow up. Number of prior debridements was used to create a sample representative of the average chronic wound patient. Data were collected on demographics, comorbidities, and infectious complications.
RESULTS: This study included 436 patients, 208 in the gravity flow group (47.7%) and 228 in the pulsatile flow group (52.3%). There were no differences in Charlson Comorbidity Index (CCI), body mass index, and hemoglobin A1c between the groups. The most common comorbidities were diabetes mellitus (n=257, 58.9%), peripheral vascular disease (n=227, 52.1%), and chronic kidney disease (n=55, 12.6%) with no differences between groups. Median wound area was 24 cm2 (IQR 7.1-60 cm2) with no difference between groups (p=0.772). Patients in the gravity flow group underwent a median of 1 prior debridement (IQR 0-2) while patients in the pulsatile flow group underwent 0 prior debridements (IQR 0-1, p<0.001). The incidence of prior positive cultures was similar between groups (p=0.932, Table 1). Infectious complications occurred more frequently in the gravity flow (n=22, 10.6%) versus pulsatile flow group (n=11, 4.8%). On bivariate logistic regression, patients undergoing debridement with gravity flow irrigation were found to have 2.3 times increased odds of developing an infectious complication (95% CI 1.10-4.93, p=0.027). When controlling for number of prior debridements and CCI, gravity flow irrigation remained independently associated with increased odds of infectious complications (OR 2.16, 95% CI 1.01-4.64, p=0.047).
CONCLUSIONS: In chronic wound patients, use of gravity flow irrigation leads to an increased risk of infectious complications. These findings are at odds with prior literature supporting non-inferiority of gravity flow irrigation in the acute traumatic population. The highly comorbid nature of the chronic wound population limits the generalizability of these prior studies. Studies specific to the chronic wound patient are critical to optimizing outcomes in this challenging population.
REFERENCES
1. FLOW Investigators, Bhandari M, Jeray K, et al. A trial of wound irrigation in the initial management of open fracure wounds. N Engl J Med. 2015;373(27):2629-2641. doi:10.1056/NEJMoa1508502 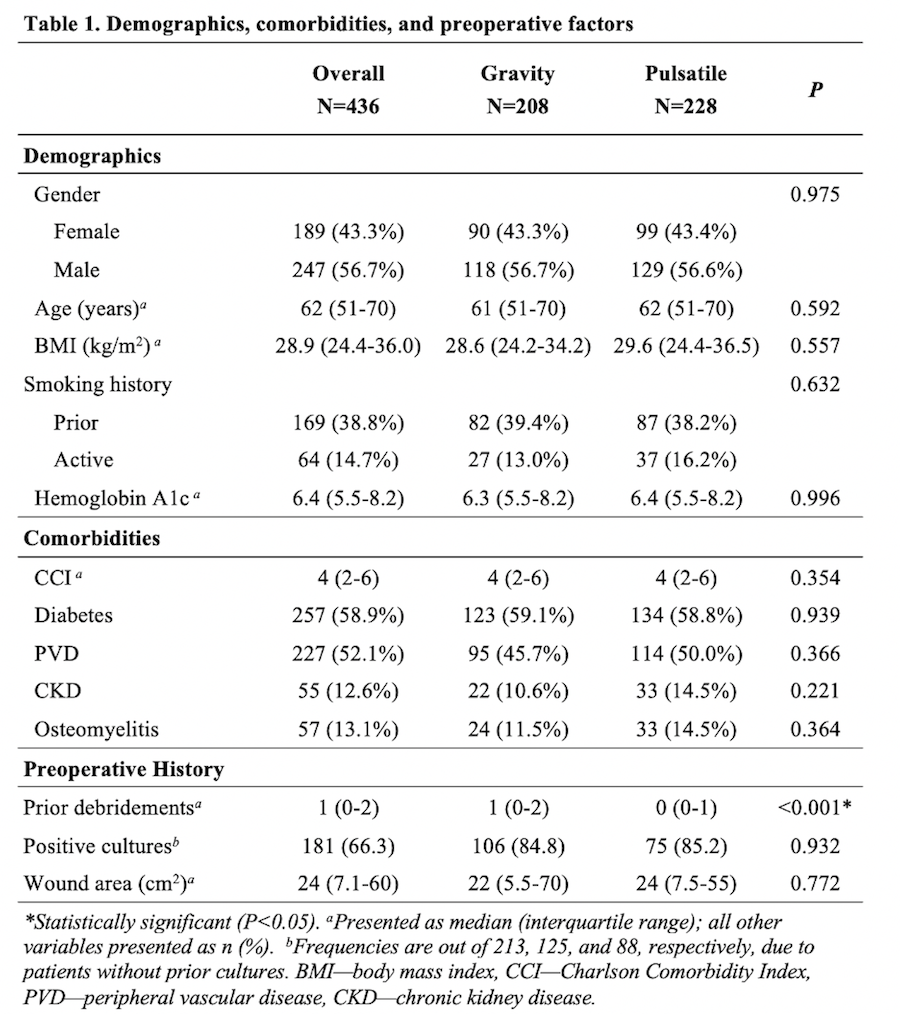
Back to 2020 Abstracts
