Virtual 3D Reduction of Displaced Mandible Fractures: A Validation Study Comparing Surgical Reductions with Virtual Reductions
Lucas A. Dvoracek, Justin Beiriger, BA, Erin Anstadt, MD, Joseph E. Losee, Jesse A. Goldstein, MD.
University of Pittsburgh, Pittsburgh, PA, USA.
BACKGROUND: Open reduction and internal fixation (ORIF) of displaced mandible fractures may lead to inadequate reduction and requires time while fixation plates are contoured. Computer-based reduction of 3D reconstructed mandible fragments and 3D printed models solves these problems by enabling plate contouring preoperatively which may guide optimal reduction. This study assesses the feasibility and characteristics of virtual mandible fracture reduction compared to surgical reduction. METHODS: Patients with displaced, noncomminuted mandible fractures who underwent ORIF and had both a pre- and post-operative CT scan were included. 3D meshes of the mandible were segmented from pre-operative and post-operative CT scans, virtual reduction of the fracture fragments was performed, and the virtually reduced and surgically reduced mandibles optimally overlayed with evaluation of qualitative and quantitative differences. RESULTS: Ten patients matched inclusion criteria (8:2 m:f, mean age 14 years). Fracture types included parasymphyseal (80%), angle (20%), body (10%), ramus (10%), and condylar (30%), and number of major fragments (excluding condyles) was 2 (80%) or 3 (20%). Virtually reduced mandibles were extremely similar to the surgically reduced mandibles, and several had improved reduction of displaced fragments. The root mean square for the average distance difference was 0.61mm (0.42-0.79, 95% CI). CONCLUSIONS: Virtual mandible reduction can yield mandibular models which are remarkably similar to surgically reduced mandibles, with the advantage of being able to manipulate the fragments freely to maximize bony contact and alignment. Models printed from this technique may enable pre-contouring of fixation plates to help guide reduction, potentially reducing malreduction, and decrease operative time. 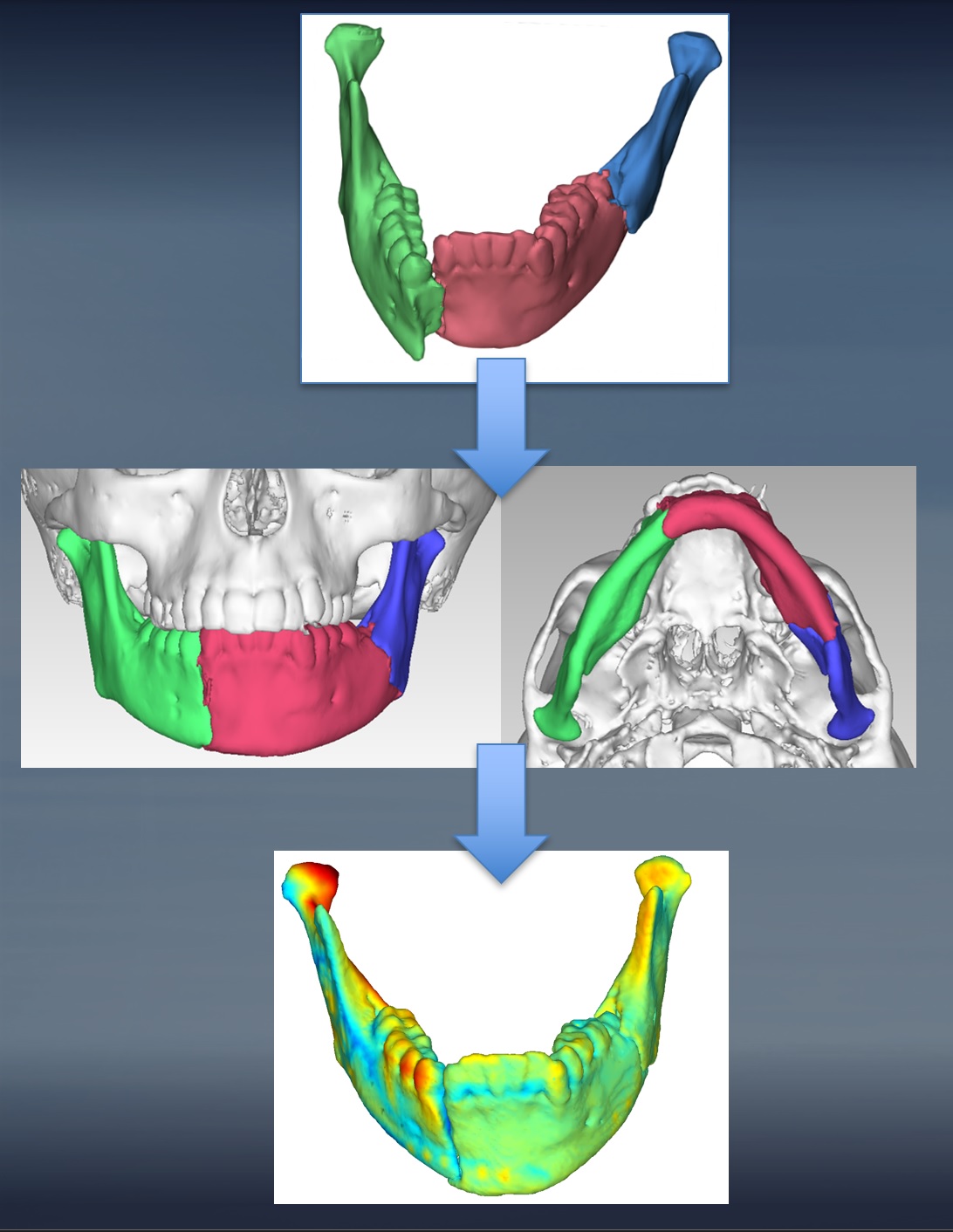
Back to 2020 Abstracts
