Ten Years of Posterior Cranial Vault Expansion via Distraction Osteogenesis: An Update and Critical Evaluation
Laura S. Humphries, MD1, Zachary D. Zapatero, B.S.1, Giap H. Vu, B.A.1, Ian Hoppe, MD2, Jordan W. Swanson, MD, MSc1, Scott P. Bartlett, MD1, Jesse A. Taylor, MD1.
1Children's Hospital of Philadelphia, Philadelphia, PA, USA, 2University of Mississippi Medical Center, Jackson, MS, USA.
Background: Over the past decade, posterior cranial vault distraction osteogenesis (PVDO) has gained momentum as primary treatment for cephalocranial disproportion associated with syndromic craniosynostosis. The goal of this study was to describe the 10-year evolution of our surgical technique, distraction protocol, and perioperative outcomes using PVDO.
Methods: A retrospective review of patients who underwent PVDO for treatment of multisuture craniosynostosis at a single institution over a 10-year period (2009 through 2019) was completed. Demographic data, perioperative outcomes, distraction patterns, and complications were analyzed. Outcomes for patients in the first 5 years of the experience (“early cohort”) were compared to those of the latter 5 years (“late cohort”).
Results: One hundred nine patients underwent a total of 117 PVDO procedures, with 8 patients requiring repeat PVDO. Syndromic patients represented 83.5% of the cohort (n=91) and were significantly younger than nonsyndromic patients at the time of first PVDO (median 15.18 [6.67, 41.82] vs 42.27 [15.18, 59.60] months, p=0.023) with a median ratio of length of follow up to years after first PVDO for the cohort of 0.90 [0.50, 1.00]. Median distraction distance in the anterior-posterior direction was 30mm (25.00, 35.00), with most patients undergoing distraction with a slight downward vector along with occipital barrel staves. Overall, 26 patients (24.78%) had 33 complications, related to either the distractor devices (n=8) or infection, CSF or wound issues (n=25), with 10 requiring re-operation for these issues. Compared to the early cohort, surgery for distractor placement in the late cohort had faster median operative times (142.50min [123.00, 186.00] vs 161.00min [138.00, 199.00], p=0.029), lower estimated blood loss as a percent of blood volume (28.30 [20.05, 44.85] vs 49.95 [31.05, 95.76], p<0.001), and lower blood replacement as percent of blood volume (39.30 [3.80, 58.20] vs 56.25 [37.75, 110.10], p=0.008). Age <12 months (p=0.029) and presence of ventriculoperitoneal (VP) shunt (p=0.036) were associated with risk for requiring repeat PVDO.
Conclusions: Our 10-year experience with PVDO demonstrates improved perioperative outcomes over time with consistent efficacy. Early complications in various subgroups, such as those with VP shunts, have led to slight technical alterations in how PVDO is performed in those groups. 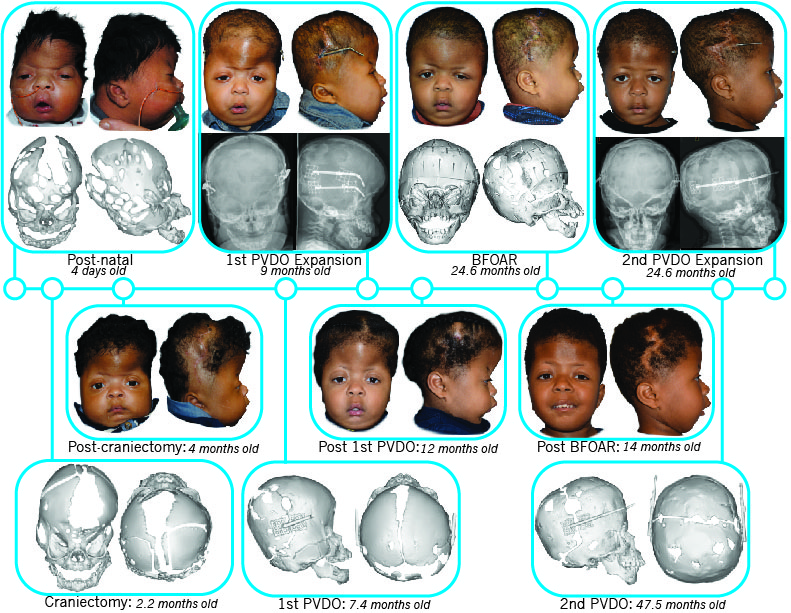
Back to 2020 Abstracts
