Estimation of Abdominal-Based Free Flap Weight in Breast Reconstruction Using a Single Preoperative Computed Tomography Scan Subcutaneous Thickness Measurement
Nicolas Greige, B.S., Bryce L. Liu, B.S., David Nash, M.D., Katie E. Weichman, M.D., Joseph A. Ricci, M.D..
Montefiore Medical Center, Bronx, NY, USA.
BACKGROUND: Estimation of the amount of free tissue available for transfer in autologous breast reconstruction is crucial for preoperative planning. Current abdominal-based free flap weight estimation methods are time-consuming and rely on multi-point computed tomography (CT) scan thickness measurements. It was our objective to develop a single-point abdominal thickness measurement formula for the estimation of abdominal-based free flap weight.
METHODS: All patients that underwent abdominal-based free tissue transfer for breast reconstruction at a single institution were retrospectively reviewed. Subcutaneous tissue thicknesses were measured on axial CT angiograms at several predetermined points: both in the midline and 5 cm lateral to midline in the plane of anterior superior iliac spine (ASIS), directly anterior to the ASIS, at the midline point equidistant from the xyphoid process and the umbilicus, and at the thickest overall point in the midline. Multivariable linear regression was used to estimate flap weight based on the single best predictor. Split-sample validation was used to internally validate the prediction model.
RESULTS: A total of 132 patients (196 flaps) were analyzed, with a mean body mass index (BMI) of 31.2 ± 4.1 kg/m2 (range: 22.6-40.7). The median intraoperative flap weight was 951 grams (IQR: 750-1186; range: 377-2250). The full predictive model (R2=0.61, n=196) estimated flap weight using the formula 16.12x+9.90y-476.74, where: x was subcutaneous tissue thickness (cm) 5 cm lateral to midline in the plane of the anterior superior iliac spine (Figure 1) and y was weight in kg. The aforementioned formula yielded a median estimated flap weight of 957 grams (IQR: 803-1198), a median percent error of 14.0% (IQR: 6.5-23.7), and a median absolute error of 122 grams (IQR: 62-231). Two-thirds split-sample validation was performed using 131 flaps to build a model and the remaining 65 flaps for validation. The training model yielded a formula 16.39x+7.67y-311.08, where x and y are as above. Upon validation we observed a median estimated flap weight of 932 grams (IQR: 842-1168), a median percent error of 12.1% (IQR: 5.2 - 19.6), and a median absolute error of 122 grams (IQR: 54-183).
CONCLUSIONS:
We developed and internally validated a simple and accurate formula for the preoperative estimation of abdominal-based free flap weight for breast reconstruction. This estimation method was validated over a wide range of flap weights and BMIs. 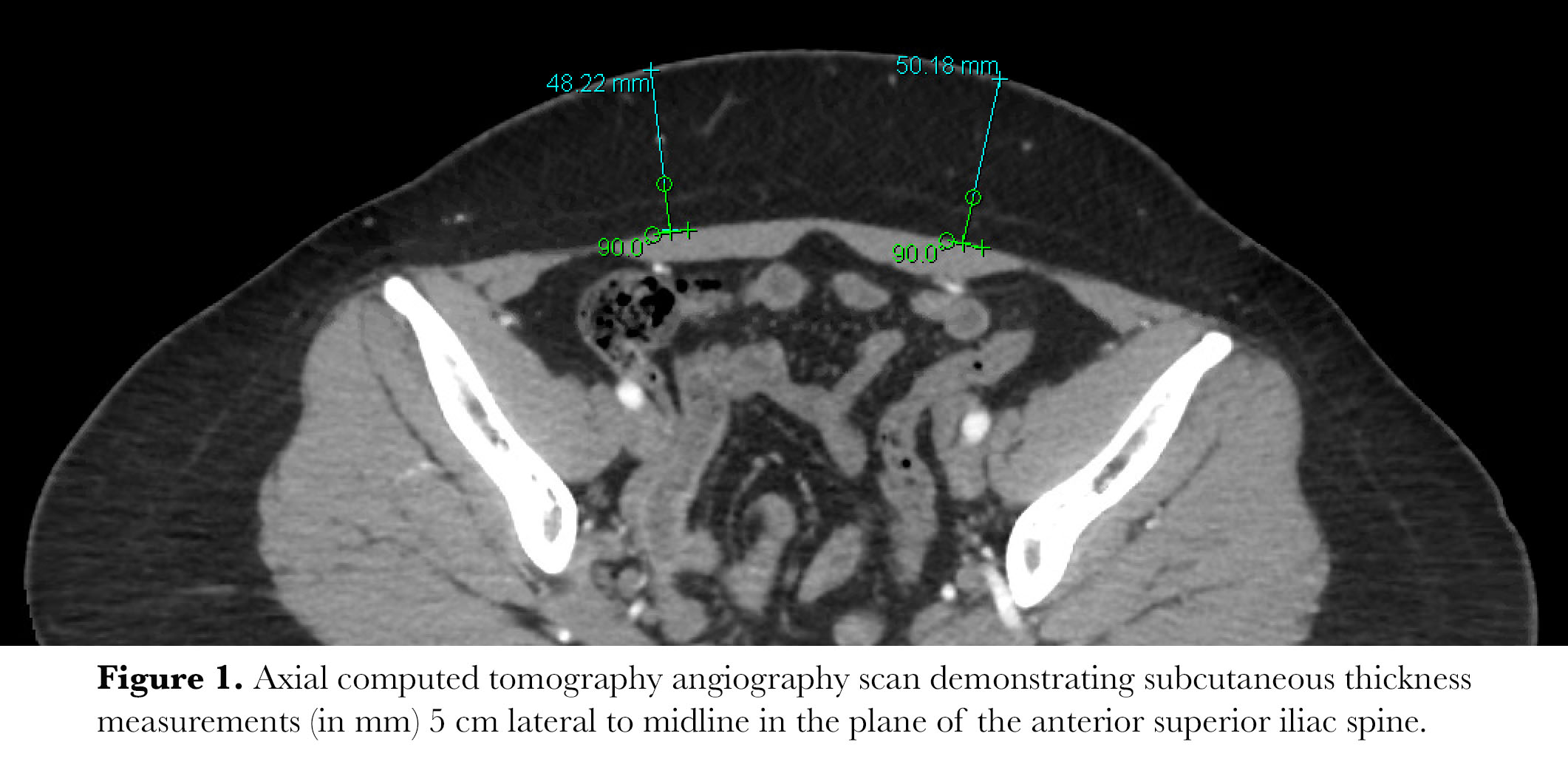
Back to 2020 Abstracts
