Frailty is the New Age: Modified Frailty Index for Preoperative Risk Assessment in Autologous Breast Reconstruction
Amanda L. Chow, BA1,2, Alexander Karius, BS1, Carisa M. Cooney, MPH1, Kristen P. Broderick, MD1
1Department of Plastic and Reconstructive Surgery, Johns Hopkins School of Medicine, Baltimore, MD, 2Division of Plastic and Reconstructive Surgery, Department of Surgery, Rutgers New Jersey Medical School, Newark, NJ
Background: Frailty has gained importance as a measure of patients' global health, particularly given the aging population. One validated preoperative assessment tool for estimating risk associated with frailty is the 5-item modified frailty index (mFI-5) which has shown to predict adverse outcomes in orthopedic, rotator cuff, and lumbar fusion surgeries. The purpose of this study was to compare mFI-5 and age as independent predictors of 30-day postoperative complications following autologous breast reconstruction.
Methods: Patients who underwent autologous breast reconstruction between 2005-2019 were identified from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). Patients were stratified based on presence of major, minor, and no complications according to the Clavien-Dindo classification. Chi-square and student's t-test were used to determine differences in mFI-5 scores between major or minor complications and no complications groups. Univariate and multivariate logistic regression were performed to determine predictability of mFI-5, age, and preoperative risk factors for major and minor 30-day postoperative complications.
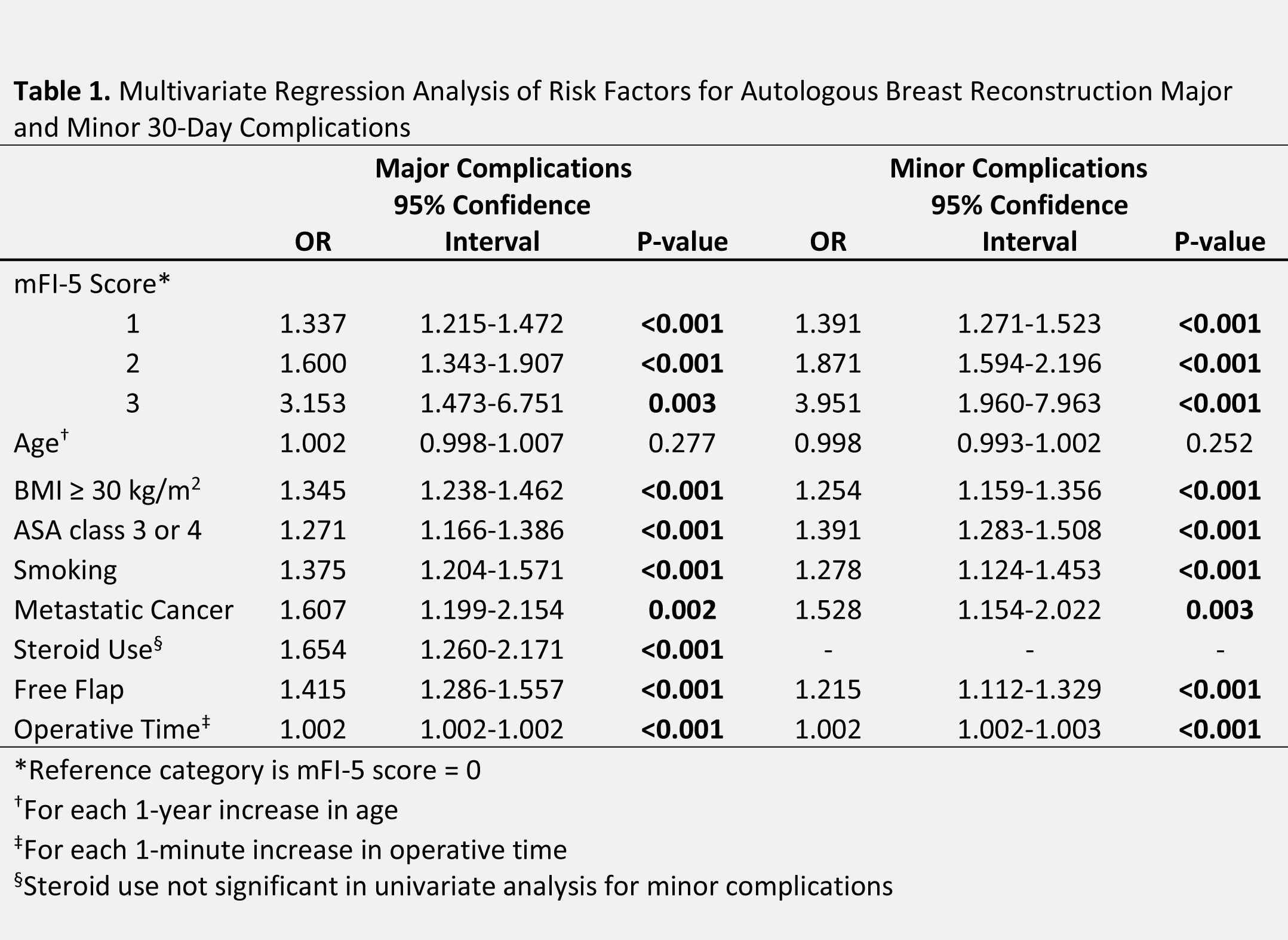
Results: A total of 25,215 patients were included, of whom 20,366 had no 30-day postoperative complications, 3,318 had minor complications, and 2,840 had major complications. Maximum mFI-5 score was 4 (n=2). mFI-5 score of 0 (n=17,788) was associated with no postoperative complications (p<0.001) while mFI-5 scores 1-3 were associated with more minor (p<0.001) and major (p<0.001) complications. Multivariate regression assessing risk factors for major 30-day postoperative complications controlling for mFI-5 score, age, obesity, ASA class 3 or 4, smoking, metastatic cancer, free flap, and operative time, demonstrated that mFI-5 of 1 (OR 1.3, p<0.001), 2 (OR 1.6, p<0.001), and 3 (OR 3.2, p=0.003) were significant predictors of major complications whereas age (OR 1.002, p=0.277) was not a predictor. Similarly, multivariate regression assessing risk factors for minor 30-day postoperative complications demonstrated that mFI-5 of 1 (OR 1.4, p<0.001), 2 (OR 1.9, p<0.001), and 3 (OR 4.0, p<0.001) were significant predictors of minor complications, and age (OR 0.9, p=0.252) was not a predictor. Higher mFI-5 was associated with increased odds of major and minor complications, with mFI-5 score of 3 nearly doubling odds of complications compared to mFI-5 score of 1.
Conclusion:: Our data demonstrate that, compared to age, mFI-5 is a better predictor of 30-day postoperative complications following autologous breast reconstruction. Additionally, higher mFI-5 scores are associated with increased odds of postoperative complications. Reconstructive breast surgeons should consider using the mFI-5 in lieu of age to risk-stratify patients prior to autologous breast reconstruction surgery.

Back to 2021 Abstracts
