Cradling the Flap: A Comparison in Outcomes Between Immediate and Babysitter DIEP Flap Reconstruction
Hao Huang BS1, Tara M. Chadab MD MS1,2, Marcos Lu Wang BA1, Sofya Norman BS1, Leslie E. Cohen MD1, David M. Otterburn MD1
1NewYork-Presbyterian, Weill Cornell Medical Center, New York, NY; 2NewYork-Presbyterian, Columbia University Irving Medical Center, New York, NY
Background: Deep inferior epigastric perforator (DIEP) flaps have become an increasingly popular modality in breast reconstruction. While DIEP flaps are commonly used to reconstruct the breast immediately after mastectomy, patients who are anticipated to undergo adjuvant radiation are not good candidates due to the risk of flap shrinkage and wound healing issues. Rather, many of these patients undergo delayed-immediate, or “babysitter,” reconstruction, where an alloplastic device is placed first as a temporizing measure during adjuvant therapy before definitive flap reconstruction. In this study, we aim to compare immediate to babysitter DIEP flap reconstruction in surgical site morbidity and other complications.
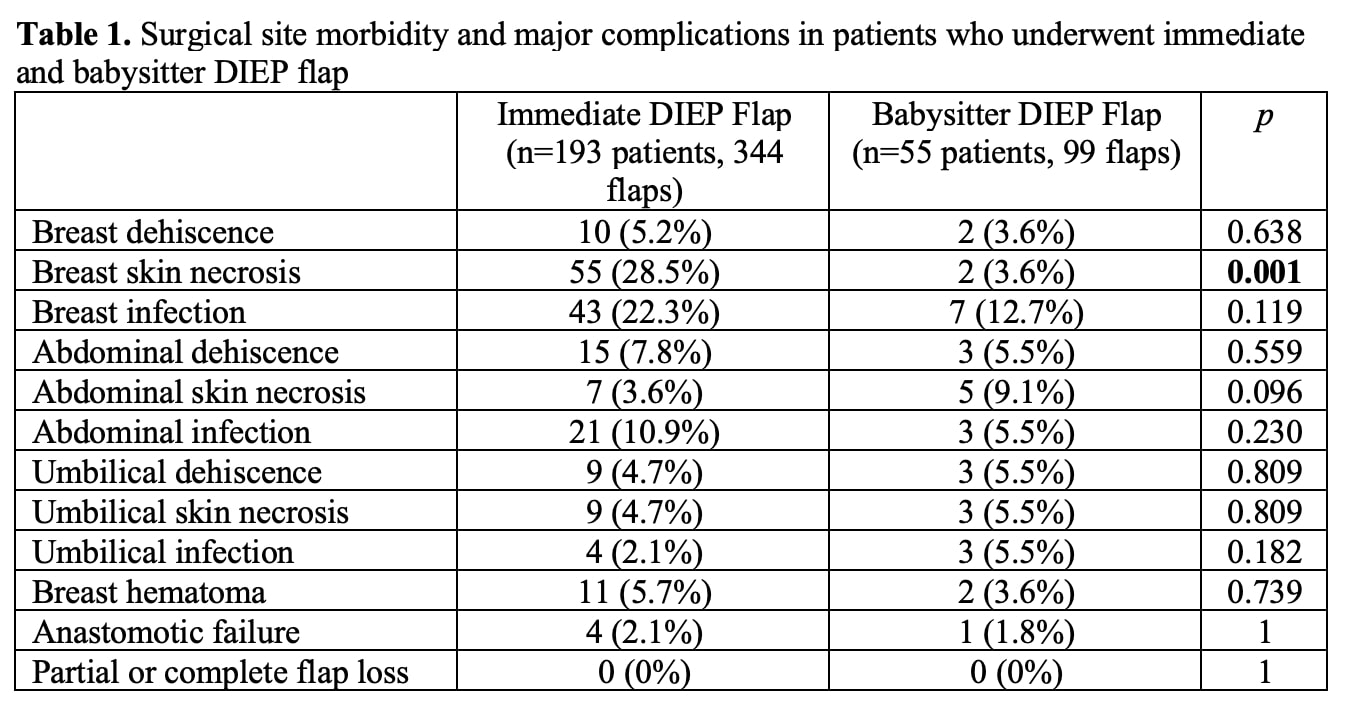
Methods: A retrospective cohort study of DIEP flap patients from August 2011 to December 2020 was conducted. Patients were divided into two cohorts: immediate reconstruction and delayed-immediate reconstruction, defined as immediate tissue expander or implant placement at time of mastectomy followed by eventual exchange for DIEP flap. Patient demographics, comorbidities, and preoperative cancer treatment were compared between the two cohorts. Clinical outcomes of interest included surgical site dehiscence, necrosis and infection. Major complications including breast hematoma, anastomotic failure, and flap loss were also noted. Results: 193 women (344 flaps) with immediate reconstruction were compared to 55 women (99 flaps) with delayed-immediate reconstruction. The two cohorts were comparable in age (50.7 vs. 50.3, p=0.780), BMI (27.2 vs. 27.2 kg/m2, p=0.996), and comorbidities including diabetes (7.3 vs. 5.5%, p=0.641) and hypertension (16.1 vs. 18.2%, p=0.709). Patients who underwent delayed-immediate DIEP flap were significantly more likely to receive preoperative chemotherapy (67.3 vs. 16.6%, p<0.001), radiotherapy (54.5 vs. 15.0%, p<0.001), and hormone therapy (72.7 vs. 10.9%, p<0.001). In terms of major complications, the immediate cohort was comparable to the delayed-immediate cohort in breast hematoma (5.7 vs. 3.6%, p=0.739), anastomotic failure (2.1 vs. 1.8%, p=1.000), and flap loss (0 vs. 0%, p=1.000). The two cohorts were also comparable in surgical site morbidity with the exception of breast skin necrosis, which was significantly higher in incidence in the immediate cohort (28.5 vs. 3.6%, p=0.001) (Table 1). Conclusions: While patients who undergo babysitter DIEP flap commonly receive adjuvant cancer treatment preoperatively, they are not at increased risk for wound-related issues of the breast, abdomen, and umbilicus. Further, they are not at elevated risk for major complications including anastomotic failure and flap loss. Delayed-immediate DIEP flap reconstruction should be considered a safe and viable reconstructive approach, especially for patients who are expected to be irradiated following mastectomy.
Back to 2021 Abstracts
