Scoring Model for Predicting Surgical Site Complications in Patients After Abdominoplasty Using National Data
Michael Coronado1, Pablo Baltodano1, Nicholas Elmer2, Briana Kaplunov1, Theresa Webster1, Karen Massada3, Rohan Brebion1, Huaqing Zhao4, Xiaoning Lu4, Sameer Patel1
1Fox Chase Cancer Center/Temple University Division of Plastic and Reconstructive Surgery, Philadelphia, PA, 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA, 3Mercy Catholic Medical Center Division of General Surgery, Philadelphia, PA, 4Temple University School of Medicine Department of Biostatistics, Philadelphia, PA
Background: Abdominoplasty complication rates are among the highest within the scope of cosmetic plastic surgery procedures. To provide a more informed and validated model of post-operative abdominoplasty care, we sought to create a scoring system that can be used to predict the likelihood of wound complications and surgical site infections using a national multi-institutional database.
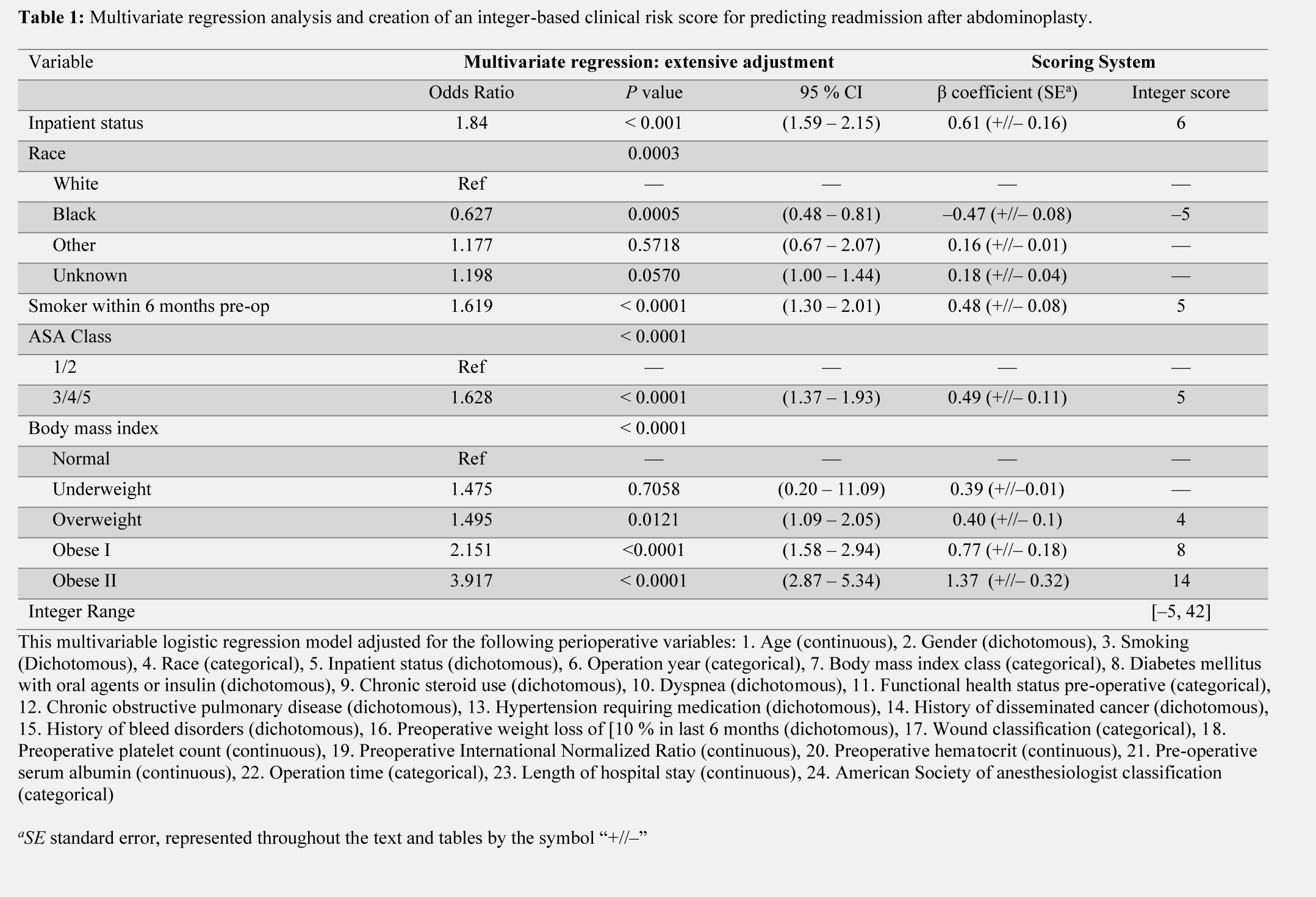
Methods: Patients who underwent abdominoplasty and those who underwent both abdominoplasty and repositioning of the belly button in the ACS-NSQIP 2007 – 2019 database were analyzed for surgical site complications defined as a composite outcome of wound disruption and superficial/deep/organ space surgical site infections. The cohort was divided into 60 and 40% random testing and validation samples. A multivariable logistic regression analysis was then performed to isolate independent factors of surgical site complications using the testing sample ( n = 11,294). The predictors were then weighted according to beta coefficients to develop an integer-based clinical risk score predictive of complications. This system was then validated using receiver operating characteristics (ROC) analysis of the validation sample ( n = 7,528).
Results: 18,822 abdominoplasty procedures were identified. 6.7% (1259/18,882) consisted of abdominoplasty with belly button repositioning. The mean (SD) age among patients within the cohort was 46.3 (12.0). 6.8% of patients developed a composite surgical site complication. Independent risk factors for composite surgical site complication included inpatient procedure (p < 0.01), smoking (p < 0.01), ASA class of 3 or higher (p< 0.01), and BMI greater than the normal range in a stepwise fashion (p < 0.01). African American race was a protective factor against surgical site complications (p < 0.01). ROC analysis of the validation cohort generated an area under the curve of 0.71, which supports the accuracy of the model.
Conclusions: This is a novel and nationally representative scoring system for predicting 30-day surgical site morbidity following abdominoplasty using data that are readily available to surgeons pre-operatively. This may allow for clinicians to screen and strategize intervention for patients considered high risk more accurately. Overall, this model serves to decrease patient morbidity and unnecessary health care expenditure.
Back to 2021 Abstracts
