The Utility of Tranexamic Acid in Aesthetic Plastic Surgery: A Systematic Review and Meta-analysis
Elizabeth Laikhter, BA1, Carly D. Comer, MD1, Paul Bain, PhD2, Eric Shiah, BA1, Samuel M. Manstein, MD1, Samuel J. Lin, MD, MBA1
1Division of Plastic and Reconstructive Surgery, Beth Israel Deaconess Medical Center, Boston, MA, 2Harvard Medical School, Boston, MA
Purpose:: Tranexamic acid (TXA) is well established for use during obstetric, orthopaedic, and cardiac surgery to prevent hemorrhage. However, its utility in plastic surgery, particularly aesthetic surgery, is limited. Therefore, this systematic review aimed to investigate the impact of TXA use in aesthetic plastic surgery on bleeding and aesthetic outcomes.
Methods: A literature search of the Medline, Embase, Web of Science, and Cochrane databases was conducted to identify all eligible studies regarding tranexamic acid use in aesthetic plastic surgery. The primary outcome of interest was intraoperative and postoperative bleeding, reported as total blood loss, ecchymosis, and hematoma formation. Data was also collected on edema, drain fluid reduction, and changes in hemoglobin and hematocrit. Meta-analyses for changes in total blood loss and postoperative hematoma formation were performed.
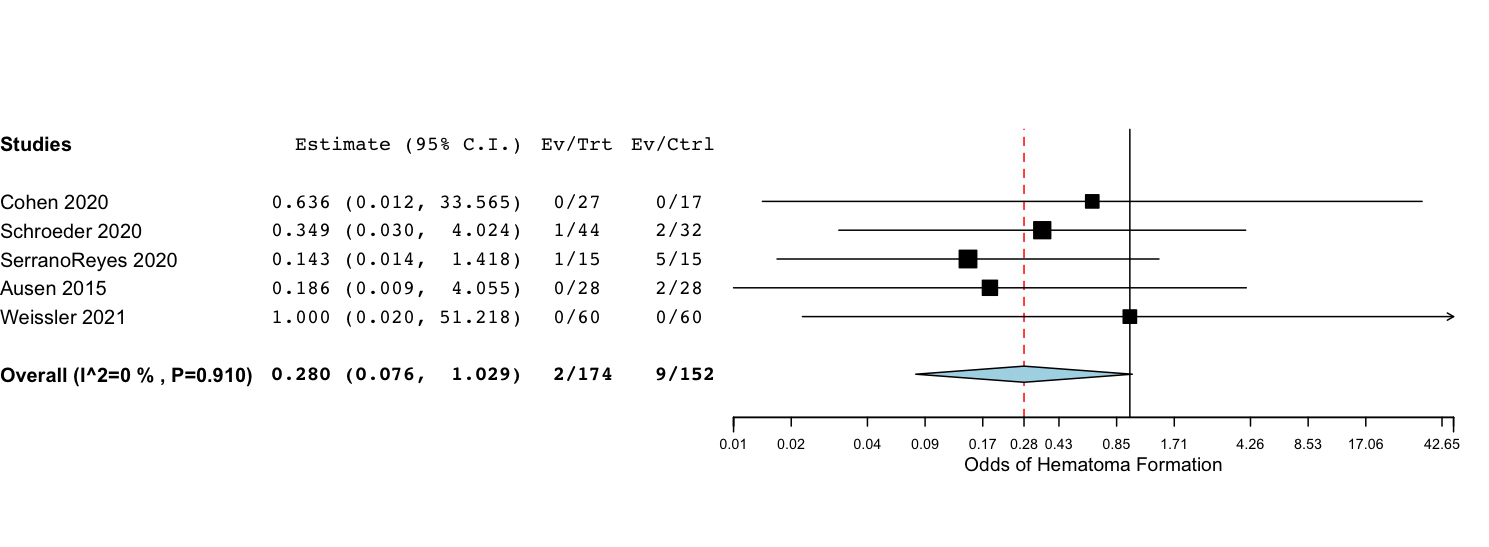
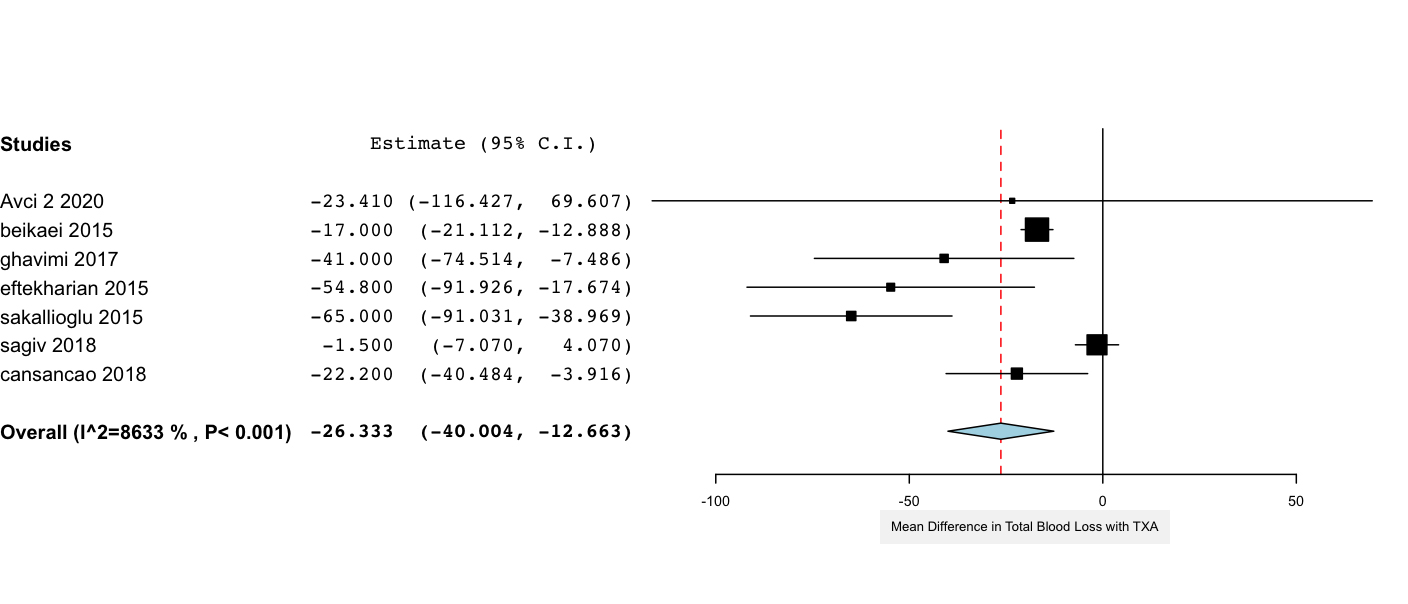
Results: Of 286 identified articles, 10 randomized controlled trials, 2 prospective cohort studies, and 2 retrospective cohort studies were included in the final analysis. The studies evaluated TXA use in reduction rhinoplasty (6), rhytidectomy (3), liposuction (3), mammaplasty (1), and blepharoplasty (1). Of 820 total patients, 446 (54.4%) received TXA. Meta-analysis of six studies reporting total blood loss demonstrated a statistically significant reduction in total blood loss by an average of 26.3 mL for patients who received TXA (95% CI: -40.0 mL to -12.7 mL, p < 0.001). Meta-analysis of five studies which explicitly noted the presence or absence of postoperative hematoma suggested that TXA is associated with a trend toward decreased odds of postoperative hematoma formation (OR: 0.280, 95% CI: 0.076 - 1.029, p = 0.055). High heterogeneity among the scoring systems for ecchymosis precluded meta-analysis; however, 5 of 7 studies found a significant decrease in the level of postoperative ecchymosis within the first 7 days after surgery. Similarly, although meta-analysis could not be carried out for postoperative fluid output, all three studies found statistically significant reductions in postoperative drain output. Notably, one study also reported significantly improved surgical site quality for patients who received TXA (p = 0.001).
Conclusions: Tranexamic acid is a low-cost antifibrinolytic agent which is associated with decreased total blood loss and a trend toward decreased bruising and hematoma formation in aesthetic plastic surgery. Its use has the potential to increase patient satisfaction with postoperative recovery and decrease costs associated with complications, such as hematoma evacuation. More studies are needed with consistent measures to perform more robust meta-analyses.
Back to 2021 Abstracts
