Critical Importance of the First Postoperative Week After Head and Neck Free Flap Reconstruction: A National Analysis of Takebacks
Nicholas A. Elmer1, Pablo A. Baltodano2, Theresa Webster3, Briana Kaplunov3, Rohan Brebion3, Karen Massada4, Mengying Deng5, Brian Egleston5, M. Shuja Shafqat2, Sameer Patel2
1Sidney Kimmel Medical College at Thomas Jefferson University, 2Fox Chase Cancer Center/ Temple University Division of Plastic and Reconstructive Surgery, 3Mercy Catholic Medical Center Division of General Surgery, Philadelphia, PA, 4Biostatistics and Bioinformatics Facility, Fox Chase Cancer Center, Philadelphia, PA
Background: Head and neck free flaps remain associated with considerable rates of takeback and prolonged hospital length of stay. However, there have been no studies on a national level benchmarking the timeline and predictors of head and neck free flap takeback. This study aims to analyze the timing and risk factors of head and neck free flap takeback on a national level.
Methods: Patients undergoing head and neck free flap reconstruction from the ACS-NSQIP 2012-2019 database were analyzed to determine the rates of takeback. Timing and rates of unplanned head and neck free flap takebacks were stratified by tissue type and post-operative day (POD) over the first month. Generalized linear models assuming log link, Gamma family, and robust standard errors were used to compare proportions over time. Multivariable logistic regression was used to identify the independent predictors of takeback.
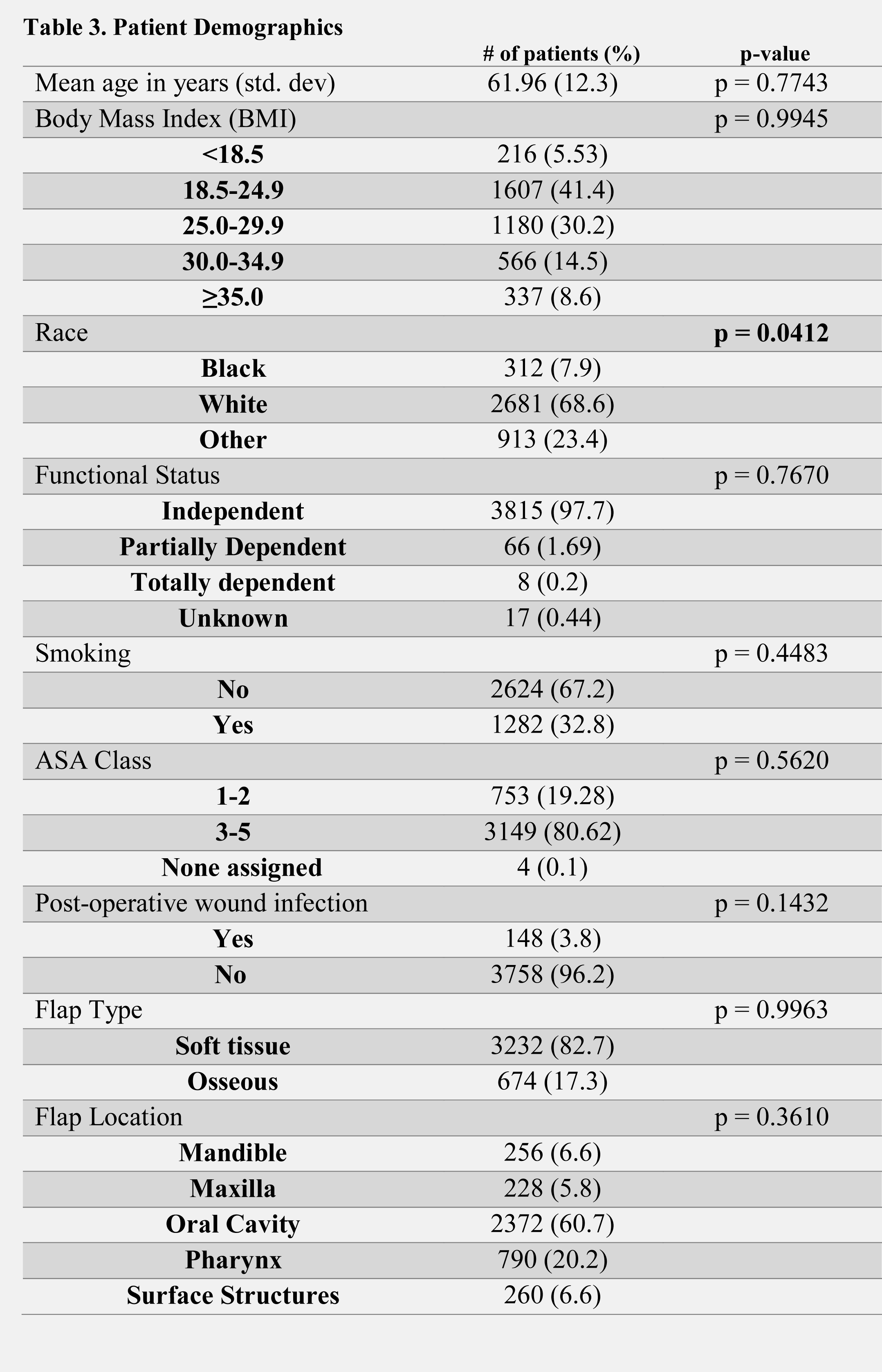
Results: 3,906 head and neck free flaps were analyzed. The mean daily proportion of patients experiencing takeback during POD 0-1 was 1.89%, this dropped significantly to a mean daily proportion of 0.54% during POD 2 (P<0.01). Additionally, a significant drop in takeback was seen comparing POD 4 to POD 5-30 from 0.2% to 0.034%/day (P<0.01). The soft tissue flap population demonstrated a similar trend in takeback. The mean daily proportion of osseous free flap takeback did not demonstrate clinically statistical significance but followed a similar trend. There was no significant difference among other flap locations and rates of reoperation. BMI, functional status, smoking status, ASA class, and presence of wound infection were not associated with increased rates of takeback. African American race (p <0.05) was found to be significant independent risk factor for takeback.
Conclusion:: This is the first national study to specifically analyze the timing of takeback in the head and neck reconstruction population. This data highlights the importance of flap monitoring during the first post-operative week; with ERAS pathway optimization aiming for discharge by the end of POD 5. Although, we acknowledge that hospital discharge depends on more factors than just the risk of takeback, based on data from this nationally validated timeline, we encourage institutions to strive to optimize their protocols and aim for discharge by the end of POD 5. This would represent a data-driven strategy to reduce the currently existing wide variability in length of hospital stay in this population.

Back to 2021 Abstracts
