Invasive Hemodynamic Monitoring in Flap-Based Lower Extremity Reconstruction: Does Monitoring Mechanism Affect Management?
Paige K. Dekker, BA2, Areeg A. Abu El Hawa, BS2, ZoŽ Haffner, BS1, Jenna C. Bekeny, MD, BA1, Kevin G. Kim, BS1, Kenneth L. Fan, MD1, Karen K. Evans, MD1
1Department of Plastic and Reconstructive Surgery, MedStar Georgetown University Hospital; Washington, District of Columbia; 2Georgetown University School of Medicine; Washington, District of Columbia
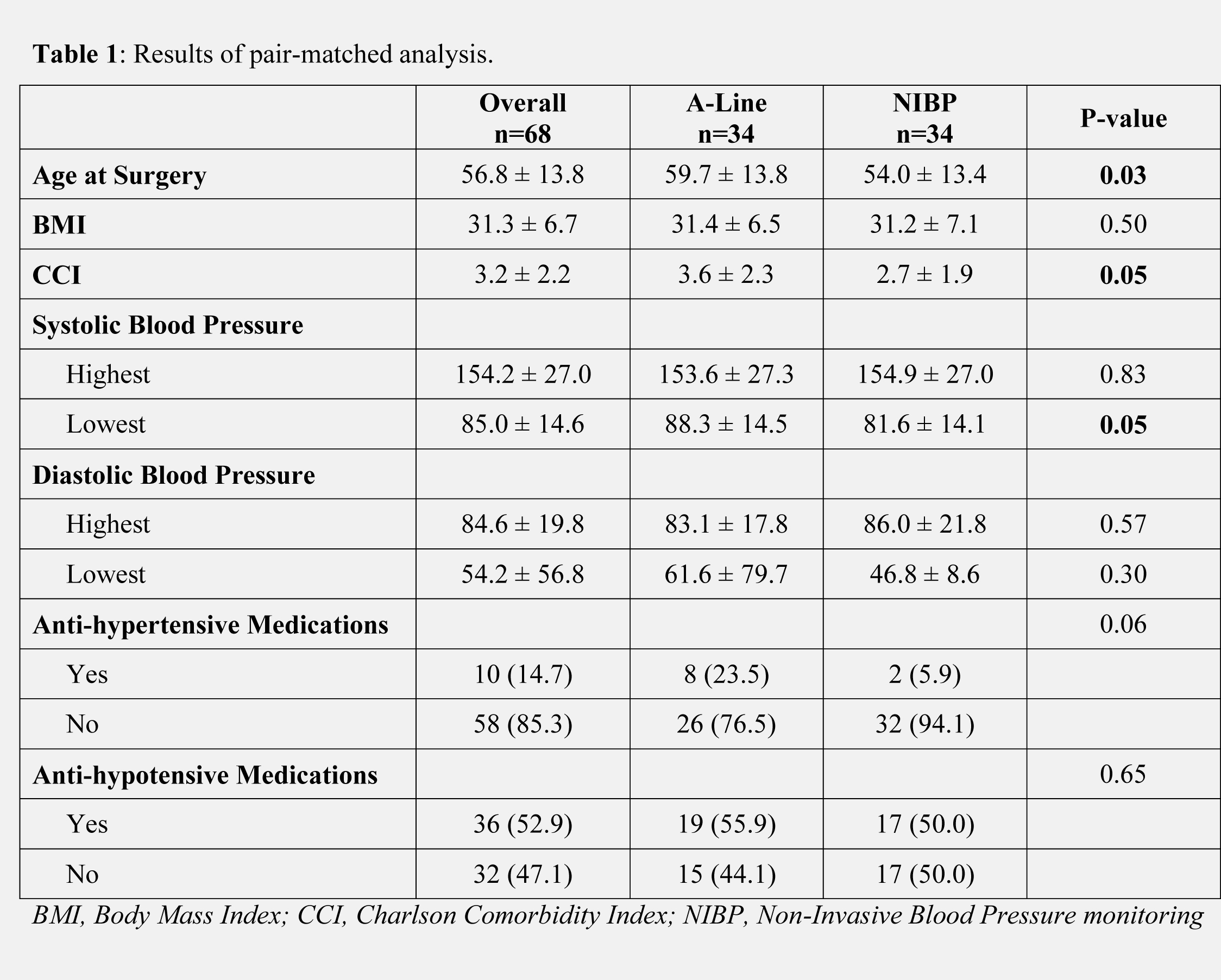
Background: There are no clear guidelines for the use of intra-arterial lines (IAL) in reconstructive cases involving free tissue transfer (FTT), but they continue to be used despite their known risks. In this study, we investigate patient factors associated with IAL placement, the relationship between hemodynamic measurements obtained via IAL and non-invasive blood pressure (NIBP) monitoring devices, and the relationship between hemodynamic monitoring method and administration of blood pressure (BP) altering medications for patients undergoing FTT for lower extremity (LE) reconstruction. Methods: All patients undergoing LE FTT at a single institution from January 2017 through June 2020 were retrospectively reviewed. Patients were pair-matched based on flap donor site, gender, BMI, and age to identify patient factors associated with IAL placement. Agreement between IAL and NIBP measurements was analyzed using methods previously described by Bland and Altman.1 Results Two groups (IAL and NIBP) with 34 patients each were included. Patients of older age and/or increased comorbidity burden were significantly more likely to have an IAL (p=0.03 and 0.05, respectively). Agreement analysis demonstrated that mean arterial pressures calculated from IAL readings ranged from 31 points lower to 28 points higher than those calculated from NIBP readings. Bias calculations with this degree of difference suggests that readings from IAL and NIBP readings are poorly correlated (R2=0.30). There were no significant differences between groups with respect to administration of BP-altering medications. Flap success rates, intraoperative complications, and takebacks were not statistically different between the two groups. Conclusion: IAL placement was associated with increased patient age and comorbidities, reinforcing the notion that the beat-to-beat monitoring offered by IAL may be useful for patients who are unable to adequately respond to hemodynamic fluctuations. Despite this, similar administration of BP-altering medications between groups suggests that intraoperative management may not be dramatically impacted by the method of hemodynamic monitoring that is used intraoperatively. Complications secondary to IAL placement are rare, but they exist nonetheless. Reconstructive surgeons should weigh the potential risks and benefits of IAL placement for each individual patient. 1. Martin Bland J, Altman DG. Statistical Methods for Assessing Agreement Between Two Methods of Clinical Measurement.Lancet.1986;327(8476):307-310.doi:10.1016/S0140-6736(86)90837-8.
Back to 2021 Abstracts
