A Novel Funnel Conduit for Improved Nerve Coaptation Outcomes Post-Traumatic Upper Extremity Injury
Erica Lee, MS, Alison Wong, MD, Sai Pinni, BS, Nicholas von Guionneau, MBBS, Thomas G.W. Harris, MBChB, Ruchita Kothari, BS, Michael Lan, BME, Bruce Enzmann, BS, Chenhu Qiu, BS, Anson Zhou, BME, Jaimie Shores, MD, Alban Latremoliere, MD, Lintao Qu, PhD, Ahmet Hoke, MD, PhD, Hai-Quan Mao, PhD, Sami Tuffaha, MD
Johns Hopkins School of Medicine, Baltimore, MD, USA
Background: Targeted muscle reinnervation (TMR) has emerged as a promising approach for the prevention and treatment of neuromas. However, the significant size-mismatch inherent to TMR contributes to substantial axonal escape from the coaptation site and consequently patients rarely achieve full resolution of symptoms. To address this limitation, we developed a funnel-shaped conduit to mechanically guide the regenerating axons across the repair site and thereby prevent axonal escape. Given the limited capacity of the distal nerve stump to accept axons regenerating from the larger proximal nerve, we incorporated chondroitin sulfate proteoglycans (CSPGs) within the lumen of the conduits to inhibit a portion of the regenerating axons. We applied the funnel conduit with and without CSPGs in a TMR model to assess the impact on functional recovery and neuroma formation.
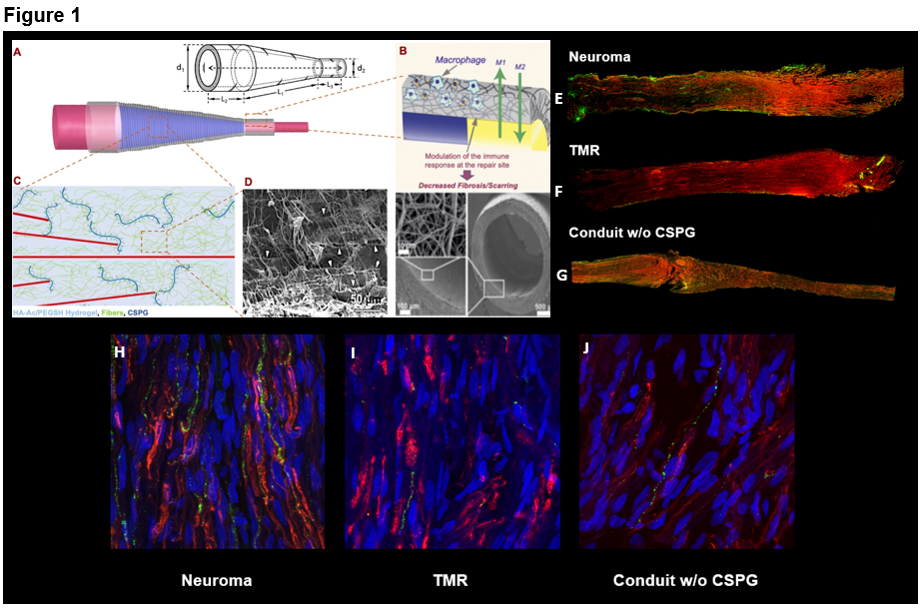
Methods: A conduit device composed of nonwoven poly-E-caprolactone (PCL), was developed by electrospinning (Figure 1A). The conduit walls prevent intraneural macrophage infiltration and inflammation, which limits scarring and fibrosis at the coaptation site (Figure 1B). Within the conduit, CSPGs incorporated into a nanofiber hydrogel form an interpenetrating network (Figure 1C, 1D). Using a TMR rodent hindlimb model, we tested the effects of this device on neuroma formation, axonal growth, muscle reinnervation, and functional recovery.
Results: Qualitative assessment of the coaptation site showed that the significant size mismatch between the sciatic nerve and tibial branch to the lateral gastrocnemius muscle resulted in neuroma formation in the TMR and neuroma groups, while the use of the conduit resulted in tapered reinnervation of the sciatic nerve, demonstrating the effectiveness of this device in mechanically guiding axonal growth (Figure 1E-1G). Neuroma and TMR groups demonstrated more co-labelling of Substance P (pain marker) and SCG10 (regeneration marker) than conduit groups (Figure 1H-1J). No significant differences were observed between the Positive Control and CSPG-Conduit groups in gastrocnemius muscle mass, myofibril cross-sectional area, and neuromuscular junction reinnervation. However, the Positive Control group exhibited significantly greater gastrocnemius mass than the TMR and the Negative Control groups, suggesting better axonal guidance and muscle reinnervation was enabled by the conduit. Autotomy scores of CSPG incorporated conduit scores were similar to Positive Control scores, suggesting successful prevention of neuroma formation.
Conclusions: We introduce a novel engineered device in which mechanical guidance of axons is combined with inhibition of axonal regeneration to prevent neuroma formation. This conduit presents a biologically compatible, non-invasive means by which we could optimize postoperative care of peripheral nerve injury.
Back to 2021 Abstracts
