The Utility of Fibrin Sealant with Acellular Dermal Matrix in Prepectoral Breast Reconstruction
Eric Weiss1, Martin Morris1, Adrienne Christopher1, Suhail Kanchwala1
Division of Plastic and Reconstructive Surgery, University of Pennsylvania, Philadelphia, Pennsylvania, U.S.
Background
Prepectoral breast reconstruction has become increasingly popular over the past decade. The resurgence in this once largely abandoned technique owes its success to the recognized benefits of modern-day breast prosthetics as well as surgical meshes, namely acellular dermal matrix (ADM). ADM bolsters the soft tissue envelope, minimizing rippling and the conspicuousness of the implant border while limiting the risk of implant exposure. Despite its utility, ADM is well known to promote seromas, leading to patient discomfort, wound complications, and infections. Fibrin sealant, a tissue adhesive substance, has widespread clinical utility. The purpose of this study is to determine whether fibrin sealant can promote ADM integration following mastectomy.
Methods
A retrospective review of consecutive patients undergoing two stage prepectoral implant-based breast reconstruction with ADM and fibrin sealant was conducted from 2018-2021. Rates of complications were assessed including seroma, hematoma, SSI, skin necrosis, prosthetic extrusion. In a separate group of patients undergoing staged autologous breast reconstruction over the same time period, ADM with fibrin sealant was utilized with prepectoral tissue expander placement following mastectomy. During the second stage, the ADM was removed and sent to pathology for histologic assessment prior to autologous delayed tissue transfer.
Results
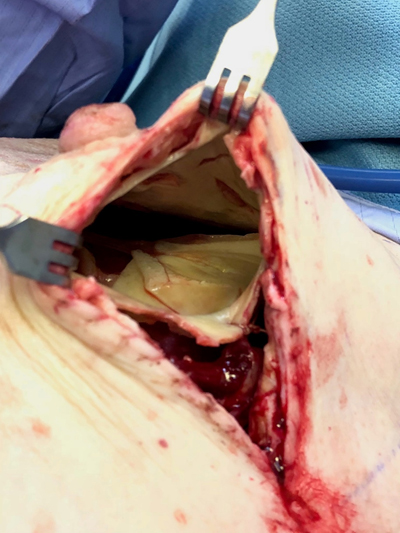
Forty-four patients underwent 79 prepectoral breast reconstructions. The overall rate of complications was 22.8%. 50% of complications were due to mastectomy flap necrosis, and 80% of these were successfully salvaged. 5.1% developed seromas requiring a single aspiration following drain removal. The rate of surgical site infection was 7.6%, the majority of which were managed with antibiotics. Among all seven patients undergoing staged autologous reconstruction, time between placement of ADM with fibrin sealant during stage I and re-exploration of the breast pocket during stage II was 18.3 days. In all patients, the ADM was clinically adherent to the mastectomy flap with sporadic evidence of punctate bleeding upon removal. Histologic analysis of the ADM-flap interface demonstrated an influx of inflammatory cells, collagen deposition, and neo-capillary formation replacing areas of remnant fibrin sealant.
Conclusion
Application of fibrin sealant to ADM permits immediate adherence to the subcutaneous breast envelope. Within three weeks, this initiates biologic integration and vascular ingrowth as the fibrin is replaced with native tissue. Clinically, use of fibrin sealant with ADM in prepectoral breast reconstruction does not increase complications and may lead to fewer seromas and earlier development of a mature breast capsule.




Back to 2021 Abstracts
