Alpha Defensin-1 Biomarker Outperforms Culture in Diagnosing Breast Implant-Related Infection: Results from a Multicenter Prospective Study
Marten N. Basta MD1, Colin White-Dzuro, BA2, Vinay Rao, MD1, Paul Y. Liu, MD FACS1, Daniel Kwan, MD1, Karl H. Breuing, MD FACS1, Rachel Sullivan, MD1, Leonard Mermel, DO3, Brian C. Drolet, MD FACS2, Scott Schmidt, MD1
1Brown University Plastic Surgery Department, Providence, RI, USA, 2Vanderbilt University School of Medicine, Nashville, TN, USA, 3Brown University Infectious Disease Department, Providence, RI, USA
Background: Prompt, accurate diagnosis of breast implant infection is critical to minimizing patient morbidity. Bacterial culture false-negative rate approaches 25-30%, and better, cost-effective testing modalities are needed. Alpha defensin-1 (AD-1), a neutrophil-mediated biomarker for infection, has replaced culture as the preferred diagnostic modality for orthopedic periprosthetic infection with sensitivity of 97%. A recent pilot study demonstrated AD-1 feasibility in breast implant-related infection. This prospective, case-control study compares the diagnostic performance of AD-1 to bacterial culture in suspected breast implant-related infection.
Methods: An IRB-approved, prospective multicenter study was conducted including adults with prior breast prosthetic reconstruction. Patients with suspected periprosthetic infection requiring operative intervention were classified as cases, while those undergoing routine expander/implant exchange or reconstructive revision were deemed controls. Implant pocket fluid was collected and analyzed with bacterial gram stain and culture, AD-1 assay, and adjunctive markers (CRP, lactate, and cell differential). Demographics, operative history, prosthetic characteristics, and antibiotic exposure were collected. Standard summary statistics were performed and univariate tests of association were conducted via Fisher exact test (categorical variables) or Wilcoxon ranksum test (continuous variables). Diagnostic test performance was assessed via sensitivity, specificity, receiver operator curves (ROC), and accuracy via Area Under the Curve (AUC), with p<0.05 considered significant.
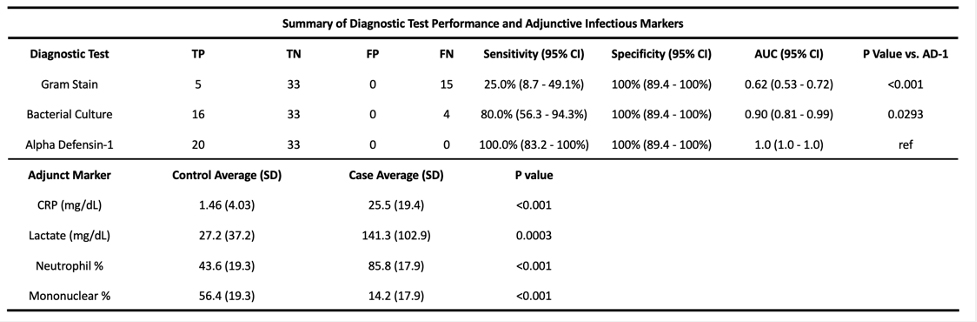
Results: Of the 53 prosthetic-based breast reconstructions included, 20 were infected and 33 controls. Age averaged 55.3 years at time of enrollment. Among 33 controls, operative indications included: 22 (67%) expander/implant exchange, 8 (24%) implant removal, 3 (9%) superficial wound debridement without signs of infection. All 20 infections demonstrated cellulitis, 13 (65%) had abnormal drainage, and 11 (55%) were febrile upon presentation. The most commonly isolated organisms were MSSA (6), coagulase-negative staphylococcus (6), and serratia marcescens (2). All cases were AD-1 positive (sensitivity=100%). Bacterial culture failed to grow any organisms in 4 infected cases (sensitivity=80.0%, p=0.046) and gram stain was the least accurate (sensitivity=25%, p<0.001). All tests demonstrated 100% specificity. ROC curves were compared, with AUC=1.0 for AD-1, AUC=0.90 (p=0.029) for culture, and AUC=0.62 (p<0.001) for gram stain. Infection adjunctive markers (CRP, Lactate, Neutrophil-%) were all significantly higher among infections versus controls (p<0.001).
Conclusion:S This prospective, multicenter study confirms the accuracy of AD-1 in diagnosing periprosthetic breast infection, and findings suggest it may outperform bacterial culture, the current diagnostic standard of care. Although further study is warranted, implications include novel diagnostic applications, as well as informing decisions to remove or replace an implant in equivocal scenarios.
Back to 2021 Abstracts
