BREAST-Q REACT: Clinical reference values for the BREAST-Q in post-mastectomy breast reconstruction patients
Jacqueline J. Chu, BA1, Jonas A. Nelson, MD, MPH1, Colleen M. McCarthy, MD1, Carrie S. Stern, MD1, Meghana G. Shamsunder, MPH1, Andrea L. Pusic, MD2, Babak J. Mehrara, MD1
1Plastic and Reconstructive Surgery Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, NY, 2Division of Plastic Surgery, Brigham and Women's Hospital, Boston, MA
Background: The BREAST-Q is the most commonly used patient reported outcome measure (PROM) for breast reconstruction research. However, clinical implementation of this PROM has been impeded by a lack of context for scores following surgery. This study defines reference values for the BREAST-Q at discrete time points after post-mastectomy breast reconstruction and validates these values by comparing them to those from a large, multi-center North American cohort. These values were then used to generate a tool for real-time BREAST-Q score interpretation.
Methods: BREAST-Q scores were prospectively obtained in women who underwent implant or autologous tissue post-mastectomy breast reconstruction preoperatively and for 2 years following surgery at Memorial Sloan Kettering Cancer Center (MSK) from 2009 to 2017. Descriptive statistics were used to create reference values for BREAST-Q satisfaction subscales at preoperative and 6 months, 1 year, and 2 years after surgery and for BREAST-Q quality-of-life subscales at preoperative and 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and 2 years after surgery. Separate reference values were generated for implant and autologous patients. Reference values were externally validated by comparing patient characteristics and BREAST-Q scores between the MSK and the Mastectomy Reconstruction Outcomes Consortium (MROC) study cohorts.
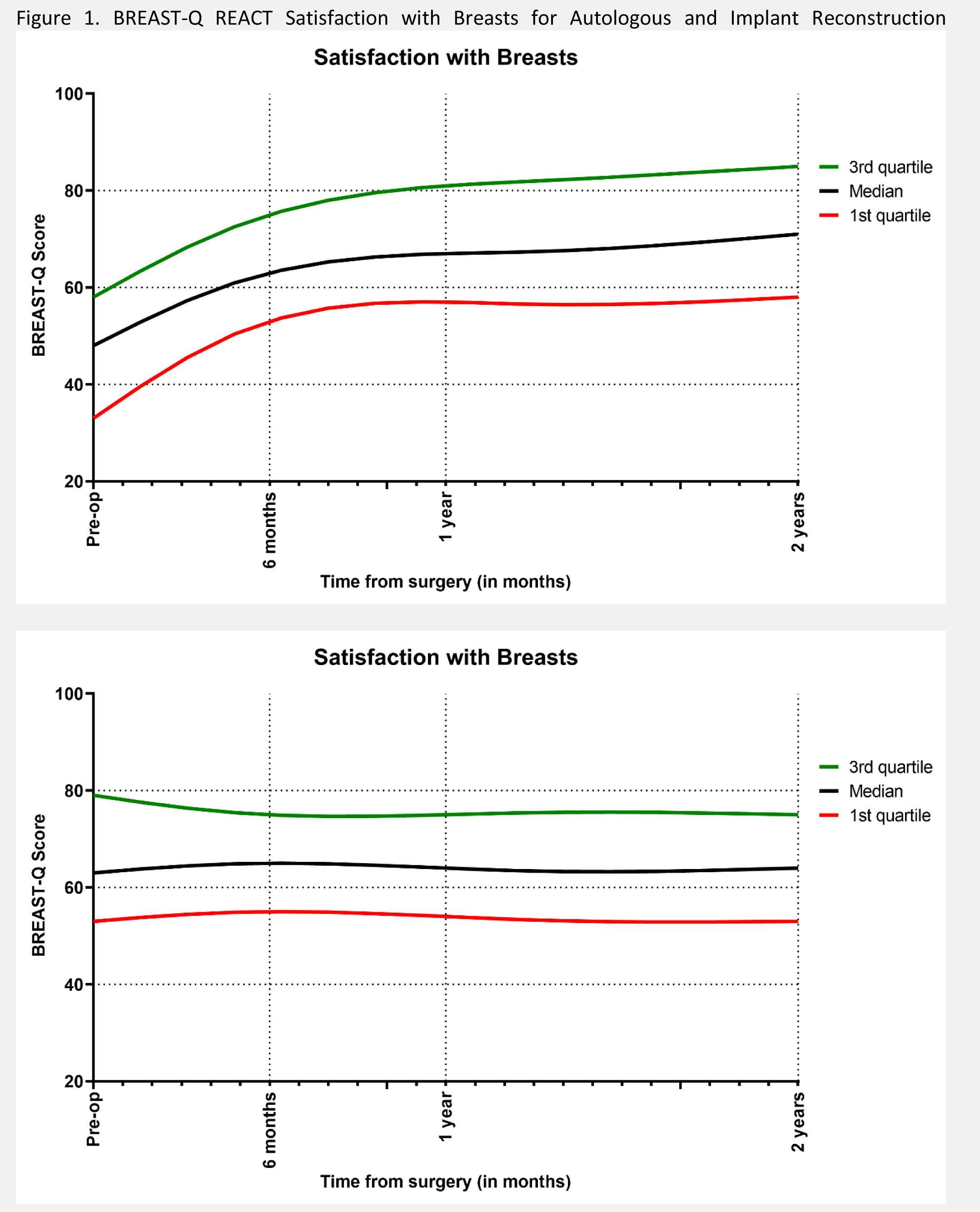
Results: Overall, 3268 MSK patients (2932 implant, 336 autologous) and 2814 MROC patients (1958 implant, 856 autologous) were included with BREAST-Q scores examined over time. Overall, few timepoint comparisons between the datasets reached clinically meaningful and statistical difference. Clinically important differences between MSK and MROC cohorts were most prevalent at 3 months after surgery, with MSK cohort patients having higher Psychosocial Wellbeing (Implants: +9.4 points, p<0.001; Autologous: +4.7 points, p=0.019) and Sexual Wellbeing (Implants: +6.1 points, p<0.001). By 1 year after surgery, differences between MSK and MROC cohorts diminished. Reference values were used to create the BREAST-Q Reconstruction Engagement and Communication Tool (REACT) for implant and autologous patients. REACT present the score trajectories for each subscale from baseline to 2 years after surgery for patients at the 25th, 50th, and 75th percentile of BREAST-Q scores.
Conclusion:: This is the first study to present BREAST-Q reference values for post-mastectomy breast reconstruction patients for use in clinical practice, with scores validated against an external, generalizable dataset. The BREAST-Q REACT will help breast reconstruction providers gauge patient wellbeing and satisfaction relative to the “average” breast reconstruction patient and determine which patients may benefit from additional intervention.
Back to 2021 Abstracts
