Semi-Automated Dermal Closure: Improved Operative Efficiency Without Sacrificing Outcomes
Martin P. Morris, MBE1, Adrienne N Christopher MD1,2, Harrison Davis, BS1, Omar Elfanagely, MD1, Robyn B. Broach, PhD1, John P. Fischer, MD, MPH1
1University of Pennsylvania, Philadelphia, PA2Thomas Jefferson University, Philadelphia, PA
BACKGROUND: With the rise in obesity in the United States, bariatric surgery and other weight loss methods have also become more prevalent. Following massive weight loss, patients are left with undesirable physical symptoms, such as excess skin. Body contouring procedures provide a solution for these patients. While many surgeons use a traditional layered suturing technique for surgical closure, the Insorb® skin stapler has gained popularity in recent years due to its ease of use as a semi-automated dermal closure (SADC) device. We aim to 1) assess the closing time and 2) determine any differences in clinical outcomes and patient-reported quality of life (PRO) scores associated with SADC.
METHODS: Patients who underwent body contouring procedures (BCP) (abdominoplasty and/or panniculectomy), or breast reduction mammoplasty (BR) by a single surgeon between 2015 – 2020 were identified by retrospective review. Patients undergoing concomitant complex hernia repair or other procedures were excluded. Patient characteristics, intraoperative details, and surgical outcomes were extracted. Cohorts were created based on surgical closure of the dermis: 1) sutures or 2) SADC. Wilcoxon rank sum tests were used to compare intraoperative closing time between the two arms. Chi squared tests were used to compare surgical outcomes. Paired Wilcoxon signed rank tests were used to compare pre- and post-operative QoL scores using validated patient-reported outcome questionnaires, the BODY-Q and the BREAST-Q.
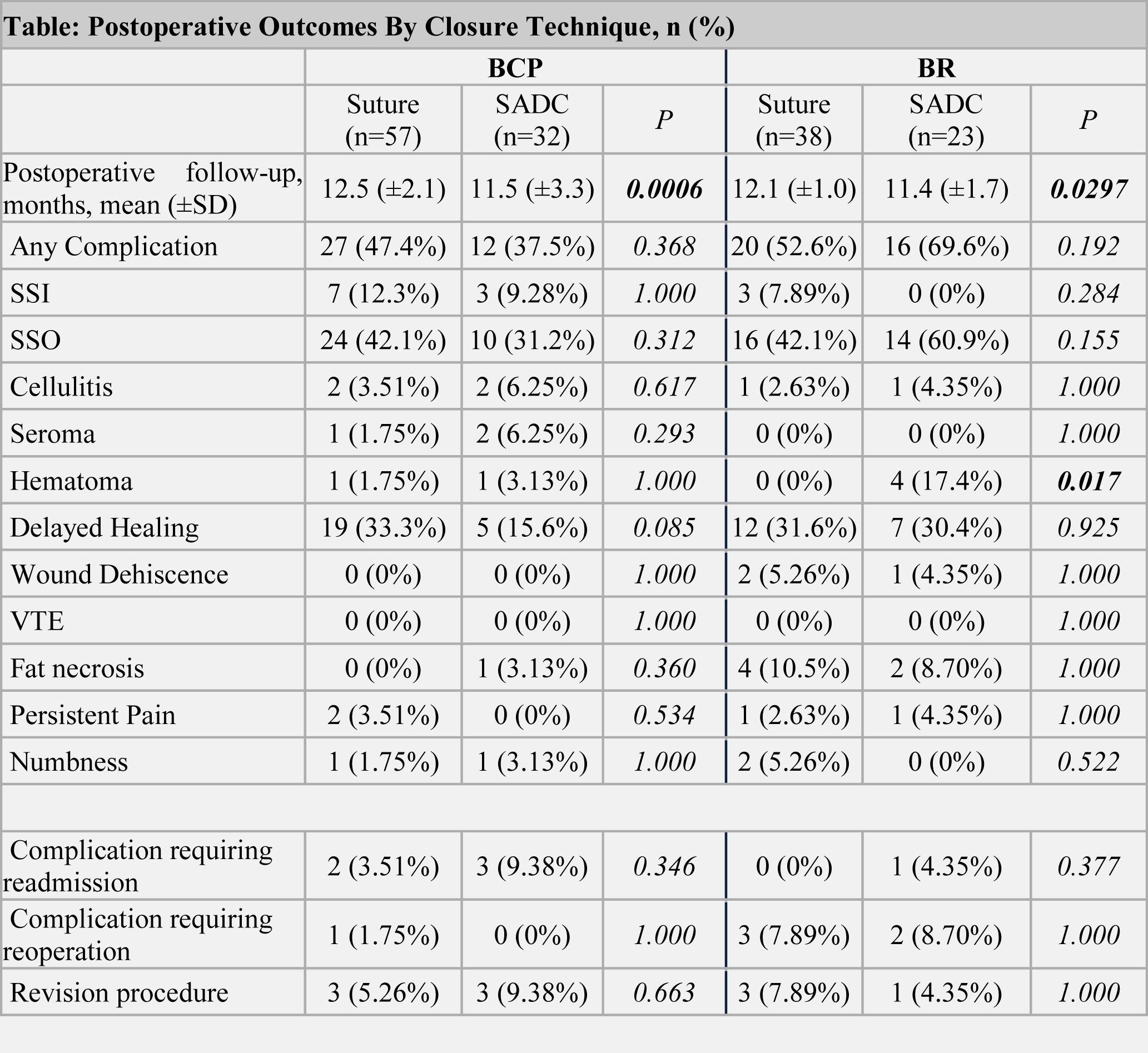
RESULTS: 103 BCP and 81 BR patients were included. Median age of the entire cohort was 42 years (interquartile range [IQR] 32-54) and median BMI was 32 kg/m2 (IQR 27-36). Use of SADC significantly decreased closure time for BCP (41 vs. 48 minutes, p=0.0262), and did not affect closure time for BR (58 vs. 59 minutes, p=0.6923). Postoperative complications were equivalent between techniques for BCP (all p>0.05). Hematoma was significantly higher in the SADC group for BR (p=0.008). All other postoperative outcomes showed no differences (p>0.05, Table 1). PROs improved across all domains for BCP and BR (all p0.05). Suture showed a greater absolute improvement of psychosocial well-being for BR (63 vs. 36, respectively, p=0.0009).
CONCLUSIONS: Use of SADC demonstrated decreased surgical closure time, postoperative clinical outcomes, and patient-reported outcomes for BCP. However, SADC use in BR showed equivalent surgical closure times, increased risk of hematoma, and decreased improvement in psychosocial well-being when compared to suture. Further exploration is needed to fully elucidate the relationship between SADC in specific plastic surgery procedures.
Back to 2021 Posters
