A Comparative Analysis of Immediate and Delayed-immediate Breast Reconstruction after Post-Mastectomy Radiation Therapy
Adrienne N. Christopher, Martin P. Morris, Robyn B. Broach, Joseph M. Serletti
Division of Plastic Surgery, Department of Surgery, University of Pennsylvania. Philadelphia, PA
Intro: Post-mastectomy radiation therapy (PMRT) is an important component in the treatment of locally advanced breast cancer. Radiation therapy, however, poses unique challenges for the reconstructive surgeon, and optimal type and timing of reconstruction in these patients is still clinically debated. Delayed-immediate autologous breast reconstruction (DI-ABR) was proposed as a two-stage reconstruction technique that would spare the definitive autologous breast reconstructionís exposure to PMRT by placing a tissue expander (TE), while also achieving some of the aesthetic and psychosocial benefits of immediate reconstruction while patients undergo adjuvant therapies with a temporary breast mound. To our knowledge, the potential risks and benefits of DI-ABR with TE compared to immediate autologous breast reconstruction (I-ABR) in the setting of PMRT has not been previously examined.
Methods: Adult patients undergoing abdominally based ABR with PMRT were separated into cohorts based on reconstructive timeline: I-ABR or DI-ABR. The groups were propensity matched 1:1 by age, body mass index, and co-morbidities. Intraoperative and postoperative surgical site events (delayed healing, seroma, hematoma, fat necrosis, skin necrosis, vascular complications, flap loss) as well as long term clinical outcomes (readmissions, reoperations, and revision procedures) were collected. In patients who had TEs prior to reconstruction, complications during radiation while TEs were in place were also collected. Univariate analyses were completed using Pearsonís Chi-square tests and Fisherís Exact tests, and statistical significance was set at p<0.05.
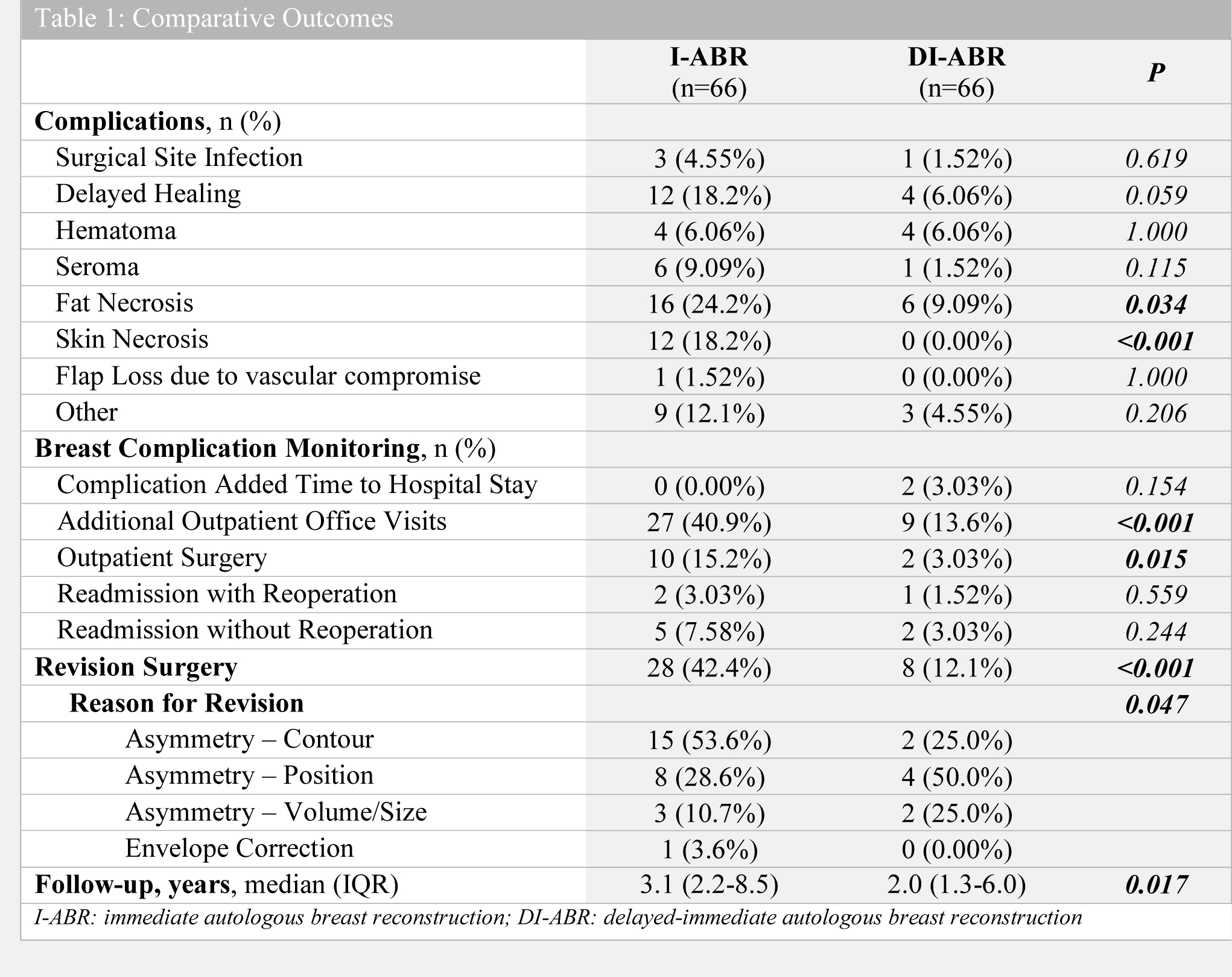
Results: 132 flaps (66 in each cohort) were identified for inclusion. Patients with I-ABR were more likely to experience fat necrosis (p=0.034), skin necrosis (p<0.001), require additional office visits (p<0.001) and outpatient surgeries (p=0.015) to manage complications, and undergo revision surgery after reconstruction (p<0.001). DI-ABR patients, however, had a 42.4% incidence of complications following TE placement, with 16.7% of patients requiring reoperation prior to reconstruction. I-ABR patients most frequently underwent revision surgery to correct breast contour, whereas DI-ABR patients were more likely to require surgery to correct the position of their breast reconstruction (p=0.047). Only one patient (I-ABR) experienced flap loss due to a vascular complication.
Conclusions: The complications encountered in both of these groups were not prohibitive to offering either treatment. Patients should be made aware of the specific and unique risks of these interventions and involved throughout the entire decision making process. Plastic surgeons should continue to strive to elucidate innovative approaches that facilitate quality of life without compromising oncologic therapy.
Back to 2021 Posters
