Impact of Nicotine Replacement Therapy on Breast Surgery Outcomes
Alexandra Junn, AB1, Jacob Dinis, BS1, Seema Patel1 Daniel Sasson1, Kaiti Duan1, Sara Islam1, Lisa Fucito, MD2, Steven L. Bernstein, MD3, Henry C. Hsia, MD1
1Division of Plastic and Reconstructive Surgery, Department of Surgery, Yale School of Medicine; New Haven, CT, USA.2Department of Psychiatry, Yale School of Medicine; New Haven, CT, USA.3Department of Emergency Medicine, Geisel School of Medicine at Dartmouth; Hanover, NH, USA.
Background: Smoking cessation therapy, including nicotine replacement therapy (NRT), is used perioperatively to assist patients in reducing tobacco smoke intake and decrease risks of smoking-associated complications. There are, however theoretical concerns nicotine-induced peripheral vasoconstriction could impair wound healing by limiting blood flow to wounds and tissue flaps. The purpose of this study is to investigate the effect of NRT on postoperative outcomes in patients undergoing breast surgery.
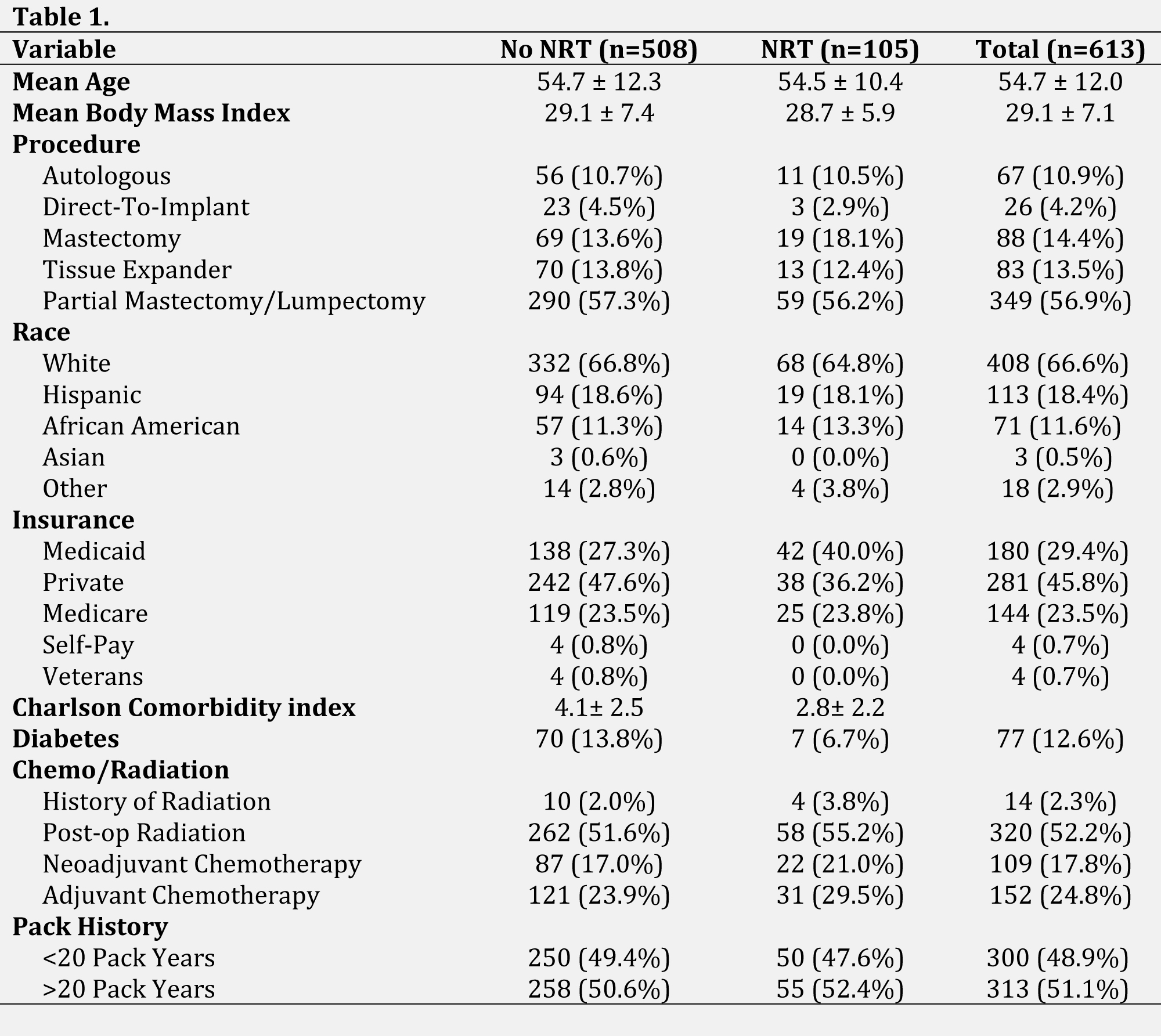
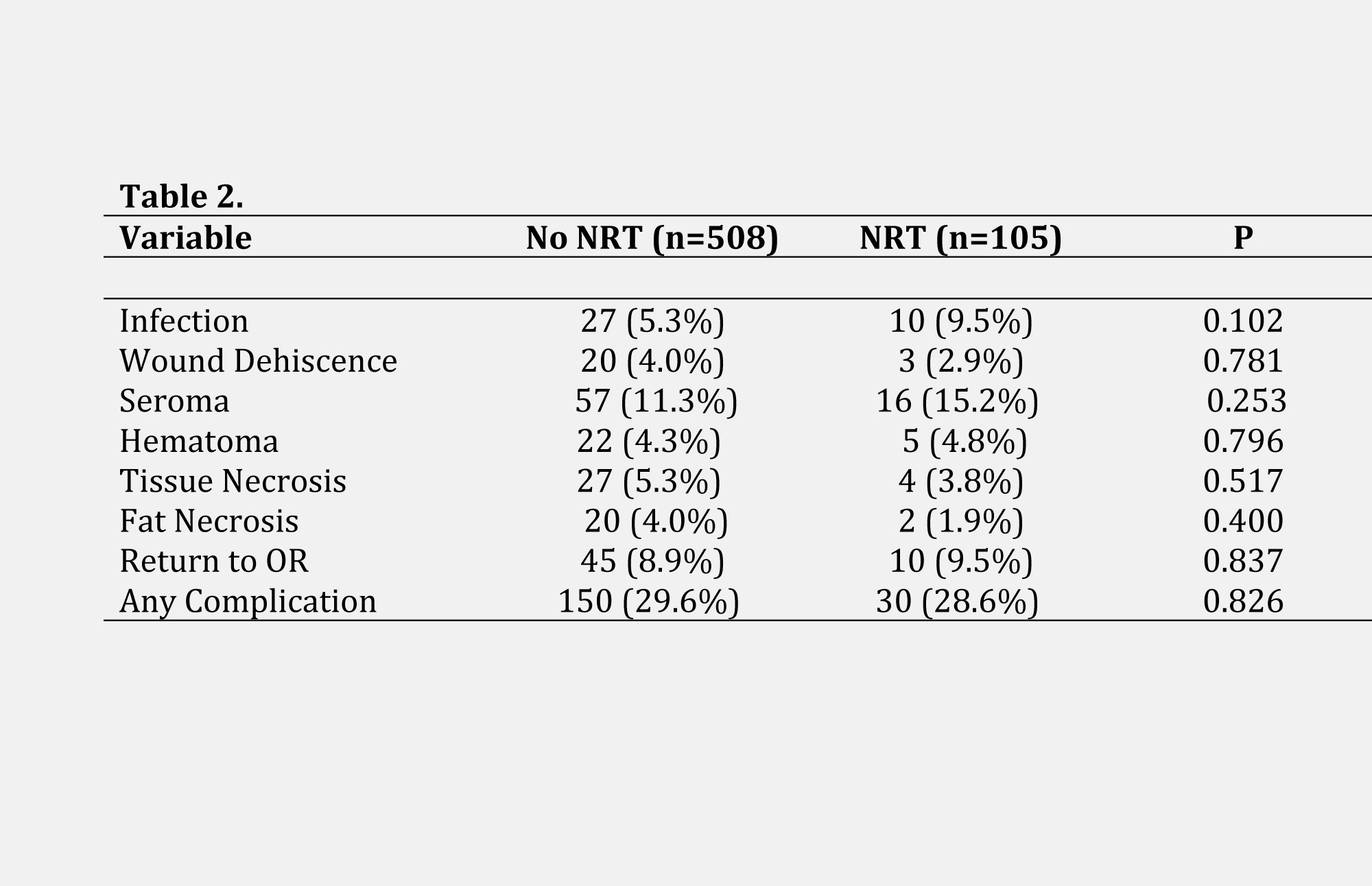
Methods: A retrospective review of all patients undergoing breast surgery at all 4 hospitals in the Yale New Haven Health System between January 2014 and December 2020 was performed. Female patients who were active smokers undergoing smoking cessation therapy prior to any of the following surgeries were included: lumpectomy/partial mastectomy, complete mastectomy with or without lymph node dissection, autologous breast reconstruction, and implant based reconstruction. Active smoking was defined as documented cigarette use during any hospital or office visit within six months before surgery. Those with documented NRT use or a prescription of NRT, whether by patch, gum, or lozenge, was noted. Small breast procedures such as excisional biopsies and nipple/areolar reconstruction, as well as patients utilizing e-cigarettes, but not combustible tobacco, were excluded. Wound complications included infection, wound dehiscence, tissue necrosis, hematoma, seroma, fat necrosis, and return to OR within 30 days. Complication data was compared between patients with NRT usage and those without using t-tests, chi-square analyses, and Mann-Whitney U tests. Multivariable logistic regression models were built to predict the effect of NRT usage on wound healing complications, and any complications.
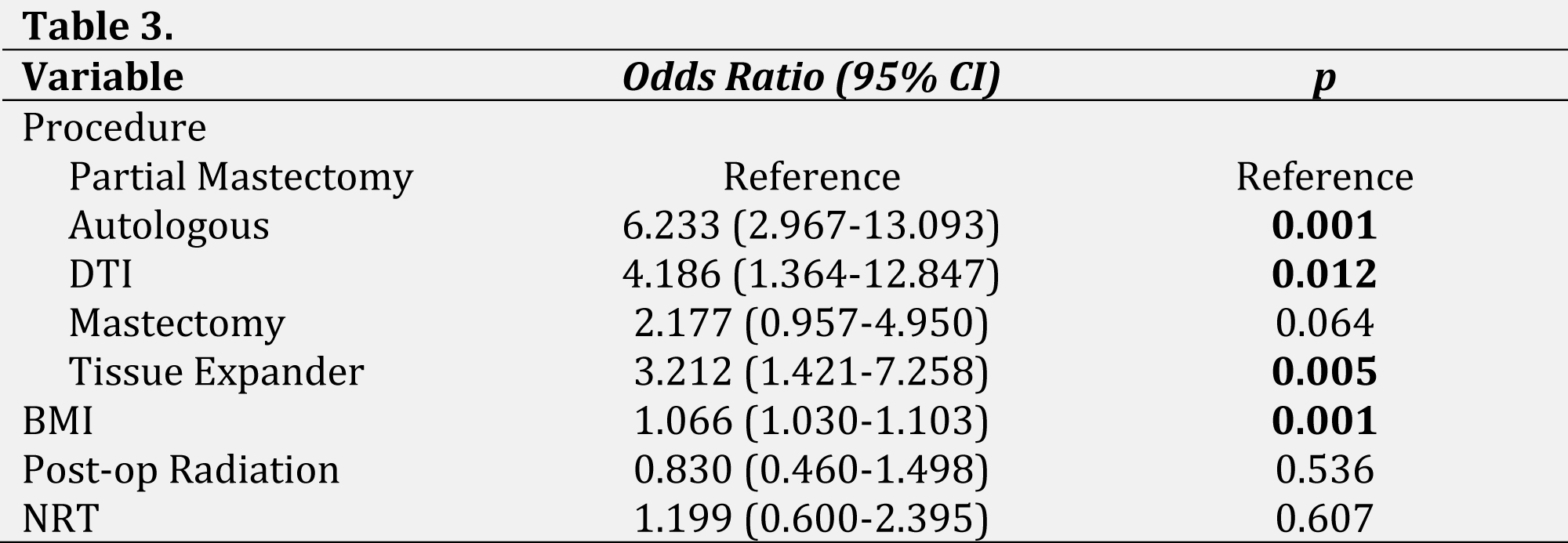
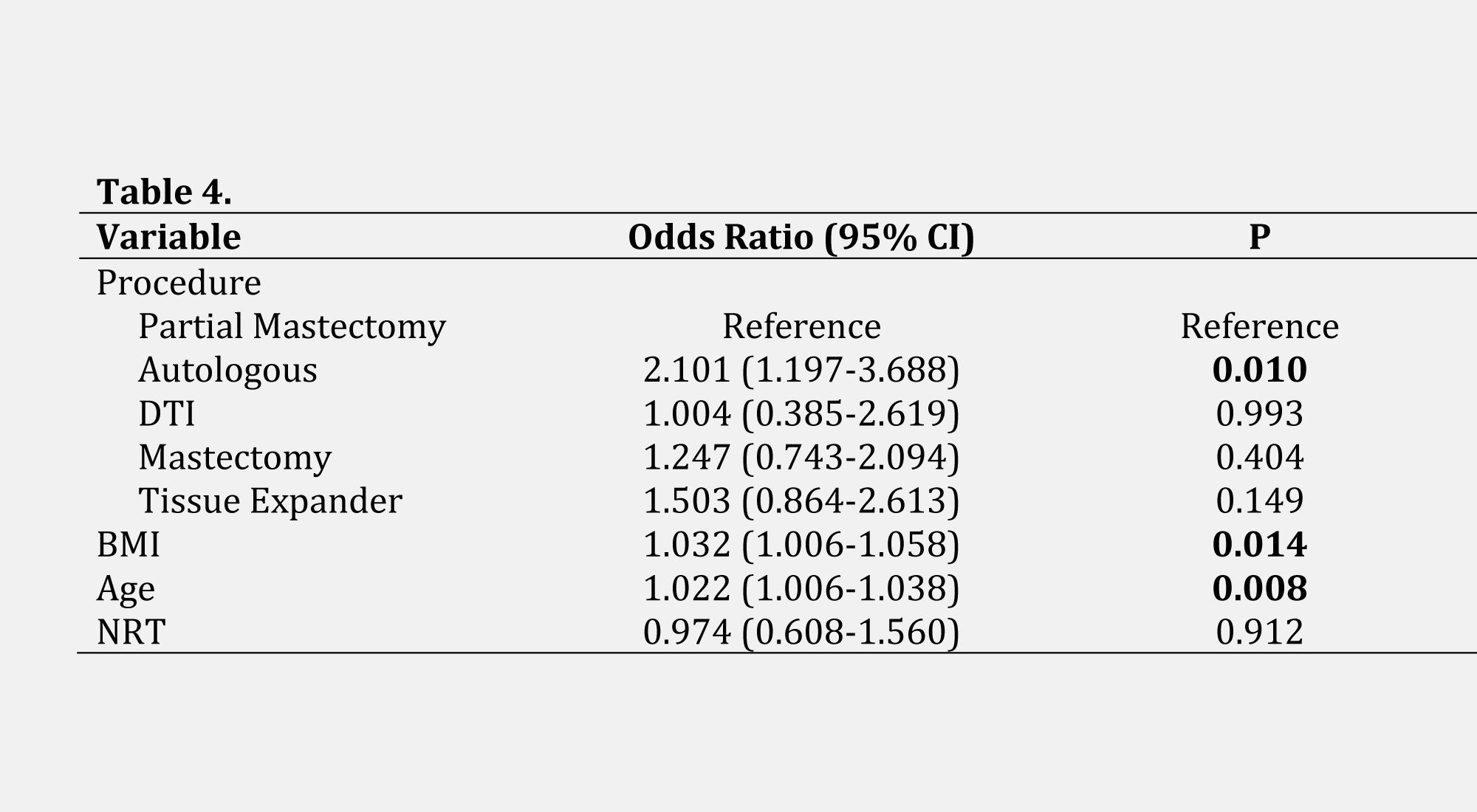
Results: 611 breast procedures met inclusion criteria, of which 105 (17.2%) had documented NRT use. No significant differences were found between the NRT cohort and the non-NRT cohort with respect to demographics. The non-NRT cohort had a complication rate of 29.6%, as compared to the 28.6% of the NRT cohort (p=0.82). Rates of infection in the NRT and non-NRT cohorts were comparable (9.5% vs 5.3%, p=0.10). In multivariable models for the risk of wound healing and any complication, NRT was not a significant predictor [OR 1.199, p=0.607; OR 0.974, p=0.912, respectively] while procedure type, increased BMI, and increased age were.
Conclusions: In this sample, NRT use was not associated with increased risk of postoperative complications compared to no NRT use for smoking cessation therapy. However, elevated BMI was associated with increased complications. Optimizing patients for surgery should focus on mitigating risk factors including obesity and smoking rather than theoretical, but clinically unverified, adverse effects of NRT.
Back to 2022 Abstracts