Phasing Out P4HB - Evaluating the Effects of Mesh Usage in Capsular Contracture Development
Yunchan Chen BS1, Marcos Lu Wang BA1, Jaime L. Bernstein MD1, Malini Chinta MD1, David M. Otterburn MD1
1Division of Plastic Surgery, Weill Cornell Medicine, New York, NY
Background: Acellular dermal matrix (ADM) and synthetic meshes are commonly used to improve inframammary-fold definition, minimize muscle excision, and allow for greater control over surgical techniques in implant-based reconstruction. However, the effect of biological and synthetic meshes on the development of post-surgical complications and capsular contracture has not been systematically explored. The aim of this study is to compare no mesh usage to the use of biological matrices (ADM) or synthetic mesh (P4HB) in conjunction with various placement locations (pre-pectoral, retro-pectoral, total sub-muscular), and further examine the respective incidences and timelines of capsular contracture development within each subgroup.
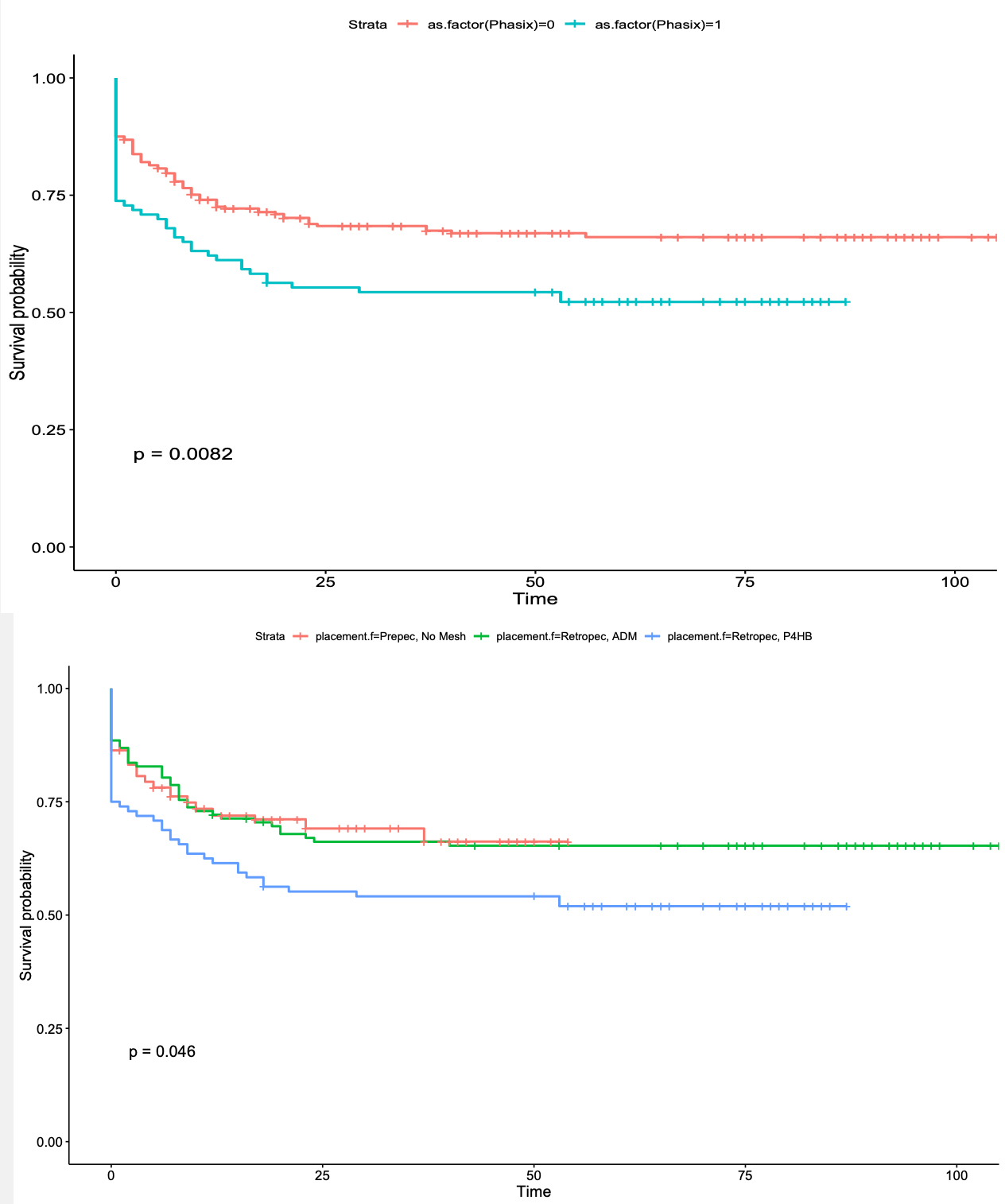
Methods: A dataset consisting of 209 patients (406 samples) who had undergone two-stage breast reconstruction between 07/20/12 - 09/17/2021 with one plastic surgeon at a tertiary-care facility was used in the study. The date of contracture development (t_c) is defined as the first mention of capsular contracture based on clinical assessment on the electronic health record. The time to event is defined as t_c - t_implant_placement_surgery if the subject developed contracture, and t_present - t_implant_placement_surgery if the subject was contracture-free. Univariate logistic regression was used for statistical analysis. Kaplan-Meier estimator was used to plot the survival curve for the various conditions.
Results: On univariate logistic regression (OR 1.95, p-value 0.004) and survival analysis (p-value 0.0082), P4HB mesh usage was linked to an increased odds of capsular contracture development. Out of the various placement modalities, retro-pectoral with P4HB yielded the highest contracture rate. Pre-pectoral placement with no mesh and retro-pectoral placement with ADM showed similar timelines of capsular contracture development. The three most common placement choices were pre-pectoral and no mesh (161/406, 39.7%), retro-pectoral and ADM (122/406, 30.0%), and retro-pectoral and P4HB mesh (96/406, 23.6%). The lowest incidence of capsular contracture occurred in the pre-pectoral placement and no mesh subgroup (49/161, 30.4%), followed by 42/122 (34.3%) and 46/96 (47.9%) in the retro-pectoral with ADM and P4HB groups, respectively.
Conclusion: The use of P4HB mesh in two-stage breast reconstruction is correlated with a statistically significant increase in the odds of developing capsular contracture. Between the three most common placement modalities, pre-pectoral tissue expander and no mesh led to the lowest rate of capsular contracture development. There did not appear to be a significant difference in the timeline of contracture formation between retro-pectoral with ADM and pre-pectoral with no mesh usage.
Back to 2022 Abstracts