Determining the Effects of Prior COVID-19 Infection on Autologous Breast Reconstruction: A Propensity Score Matched Analysis
Alexander K Karius1, Jonlin Chen1, Rafael Felix P Tiongco1, Tomer Lagziel1, Carisa M Cooney1, Kristen P Broderick1
1The Johns Hopkins University School of Medicine, Baltimore, MD
Background: Major shifts in healthcare systems worldwide have occurred due to COVID-19. With nearly half of all Americans now having a history of COVID-19 infection, there is a pressing need to better understand the importance of prior COVID-19 infection as a potential surgical risk factor. The aim of this study was to investigate the impact of a history of prior COVID-19 infection on patient outcomes following autologous breast reconstruction.
Methods: We performed a retrospective study using the TriNetX research database, which contains deidentified patient records from 58 participating international healthcare organizations. All patients who underwent autologous breast reconstruction between April 1, 2020 and January 21, 2022. were included and were grouped based on history of a prior COVID-19 infection. Demographic, preoperative risk factors, and 90-day postoperative complication data were compared. Data were analyzed by propensity score-matched analysis on TriNetX. Statistical analyses were performed by Fisher’s exact, X2 tests, and Mann-Whitney U tests as appropriate. Significance was set at p-values of < 0.05.
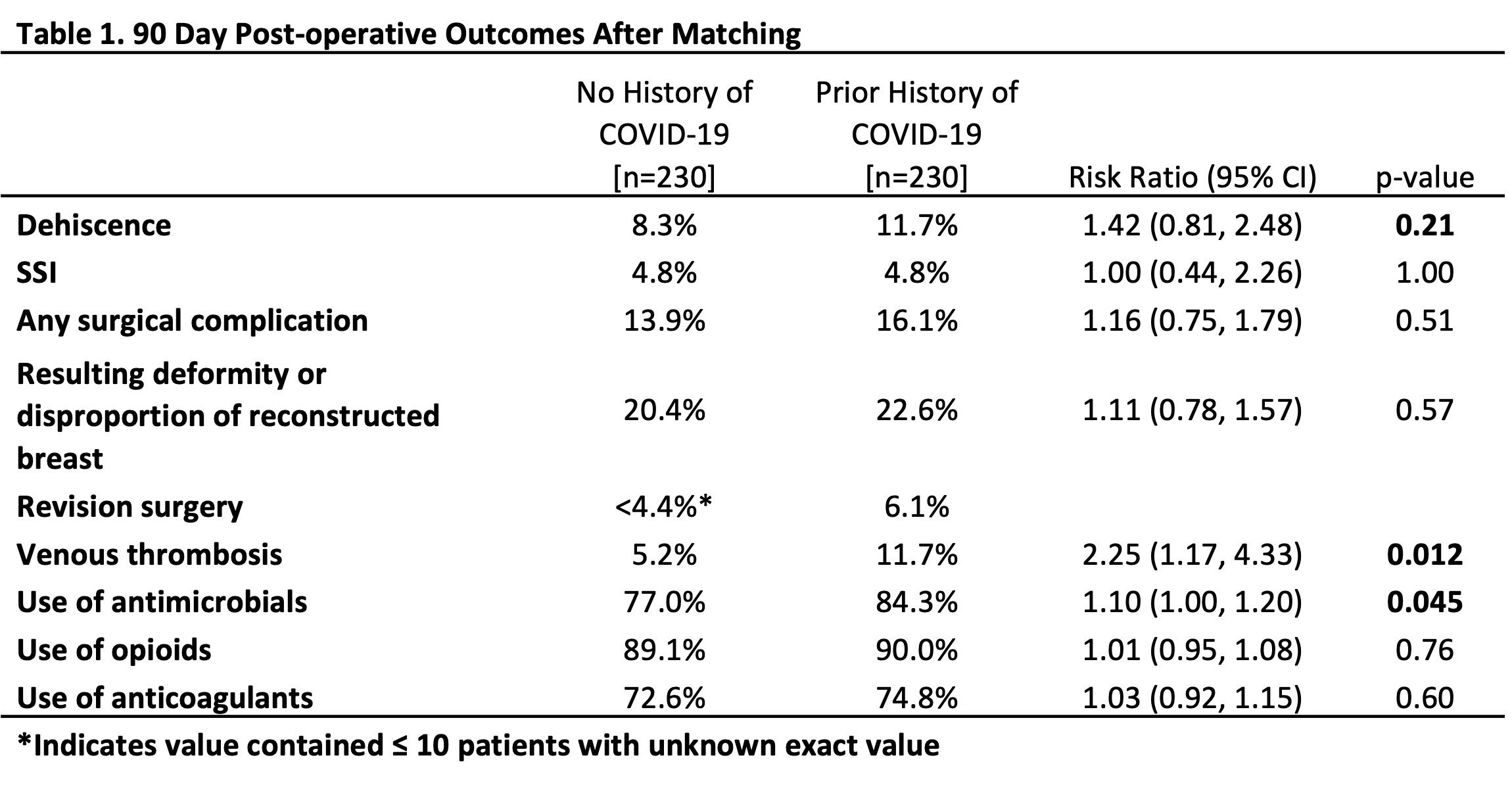
Results: Patients with a history of autologous breast reconstruction within our temporal study window (n=3,215) were divided into groups with (n=230) and without (n=2,985) a prior COVID-19 diagnosis. Non-matched patients with prior COVID-19 had increased rates of select 90-day postoperative complications, including contour deformities (22.6% vs. 16.2%, p=0.012), and thrombotic events (11.7% vs. 4.4%, p<0.0001). Use of antimicrobial medications was also found to be higher in those with prior COVID-19 (84.6% vs. 77.3%, p=0.098). After performing propensity-score matching, each cohort consisted of 230 patients without statistically significant differences between any baseline characteristics used for propensity- score matching (age, race, ethnicity, hypertension, diabetes mellitus, history of breast cancer, history of chemotherapy, and history of radiation therapy). After matching, none of the analyzed outcomes were significantly different between patients with and without a history of COVID-19, except for rate of thrombotic events, which was greater in patients with a prior history of COVID-19 (10.0% vs 4.4%, p=0.0067).
Conclusion: After propensity-score matching, only rate of thrombotic events was higher in patients with a history of COVID-19, while all other outcomes, including total rate of any complications, were similar between the two groups. Therefore, a prior COVID-19 infection is not a significant risk factor for autologous breast reconstruction complications.
Back to 2022 Abstracts