Head and Neck Cancer Care - Show Me the Money
Seth Z. Aschen1, MD, MBA, Gillian M. O'Connell2, AB, and Jason A. Spector1, MD
1Weill Cornell Medical College Division of Plastic and Reconstructive Surgery, Weill Cornell Medicine2Columbia Vagelos College of Physicians & Surgeons Division of Plastic and Reconstructive Surgery, Columbia University Irving Medical Center
BACKGOUND: The incidence of head and neck cancers (HNC) in the United States is increasing each year, with a shift in the dominant disease pathophysiology from smoking to HPV. Compared to breast cancer (BC), HNC has substantially fewer support groups (2 versus 8), tax-exempt organizations (11 versus 639) and grant funding ($75 million versus $614 million). Reimbursement for procedures is an important determinant of availability and access to care. This study compares reimbursements for comparable reconstructive procedures in HNC and BC patients. Additionally, hospital charges and costs associated with caring for patients in both groups were compared.
METHODS: Pricing data was abstracted from the Centers for Medicare and Medicaid Services Physician Fee Schedule Look-Up Tool. Reimbursement data for CPT codes 15757, 15733, 19364 and 19367 was calculated using relative value units and the conversion factor for each CPT code of interest for fiscal years 2012 to 2021 adjusting for inflation. Studentís t-test was used to determine statistical significance. Publicly accessible patient-level data for 2015 to 2017 was acquired from the New York State Department of Health and analyzed in R Studio (v1. 3.1). HNC and BC patients admitted for procedures relating to cancer care were identified using MDC, CCS, and APR-DRG codes. Wilcoxon-Mann-Whitney tests for statistical significance were used for inter-group and subgroup analyses.
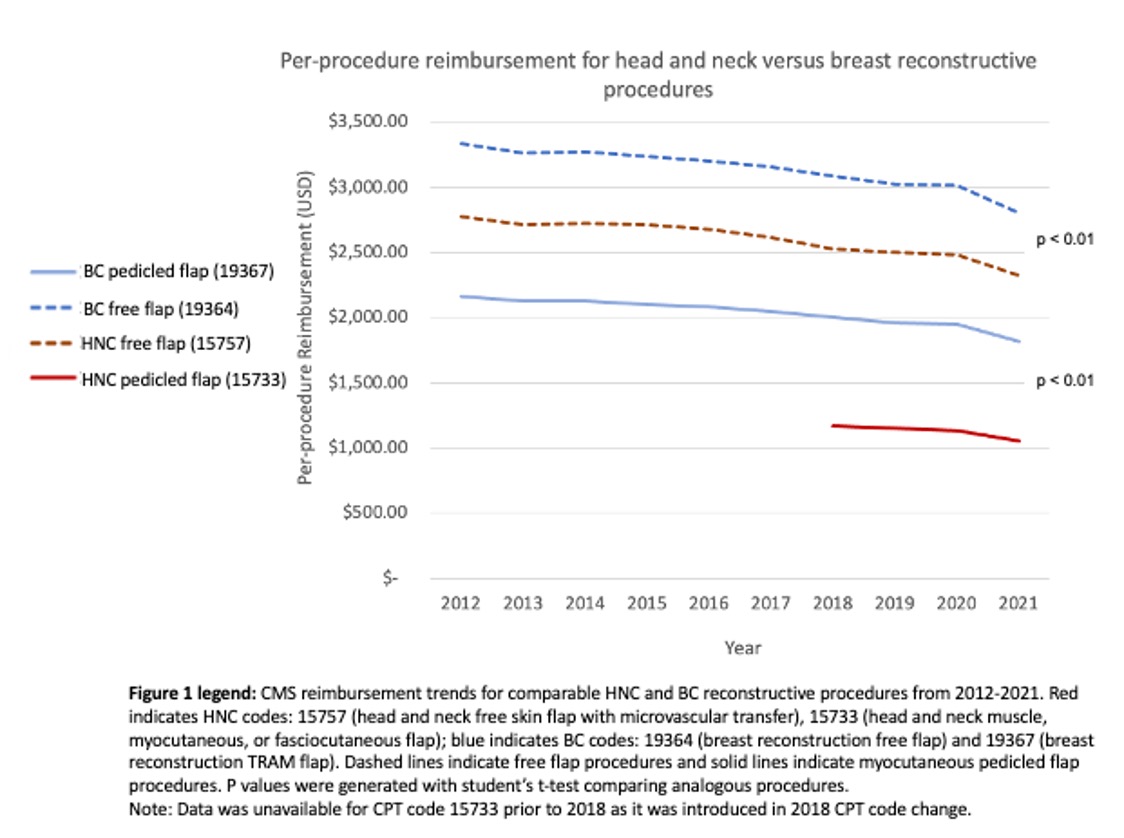
RESULTS: Comparison of procedure reimbursement for free and pedicled flaps for HNC and BC reconstruction indicated that HNC procedures had significantly lower reimbursement than BC procedures over the study period (p < 0.01) [Figure 1]. Analysis of patient data across New York State demonstrated that cancer patients hospitalized for HNC procedures were more likely to have public insurance, require longer lengths of stay, and generate higher hospital costs than patients hospitalized for BC procedures (p < 0.01). Within HNC patients, publicly insured patients had significantly longer lengths of stay and higher costs per day than privately insured patients (p < 0.01).
CONCLUSION: Reimbursement for reconstructive HNC procedures is significantly lower than that for reconstructive BC procedures of comparable work effort. Additionally, HNC patients are more likely to be publicly insured and have longer lengths of stay than patients undergoing breast reconstruction, increasing hospital costs and further widening the gap in reimbursement between these two patient groups. The large discrepancy in reimbursement may financially disincentivize investment in care for HNC patients, raising concern for future access to care in this growing patient population.
Back to 2022 Abstracts