Rectus Plication Does Not Increase Risk of Thromboembolic Events Following Abdominal Body Contouring: A Matched Case-Control Analysis
Fei Wang1, Katherine Chemakin1, Peter Shamamian1, Isha Punn1, Tessa Campbell1, Joseph A. Ricci1
1Albert Einstein College of Medicine; Montefiore Medical Center, Bronx, New York
Background: Venous thromboembolic events (VTE) such as deep venous thrombosis (DVT) and pulmonary embolism (PE) are rare but potentially devastating complications of abdominal body contouring procedures. With an incidence of around 1%, the VTE rate in these surgeries is significantly lower than that of other surgical specialties but remain a significant cause of morbidity and mortality. Rectus abdominis plication, a commonly utilized method to reduce diastasis width, has been associated with increased intra-abdominal pressure. Though concerns that this increased intra-abdominal pressure may lead to increased DVTs and subsequent PEs exist, there is a lack of literature investigating associations between the two in abdominal contouring procedures and we aim to bridge this gap in knowledge.
Methods: A retrospective review was conducted for all patients who underwent abdominal body contouring procedures at Montefiore Medical Center between 2010 and 2020. Cases were defined as patients who experienced a postoperative venous thromboembolic event and were matched to controls in a 1:4 ratio using the propensity score matching technique. Patient factors of note included demographic data, operative details, ASA, Charlson comorbidity index, and Caprini scores. Postoperative complications were collected for all patients. Parametric, nonparametric, and multivariable regression modeling was utilized for analysis.
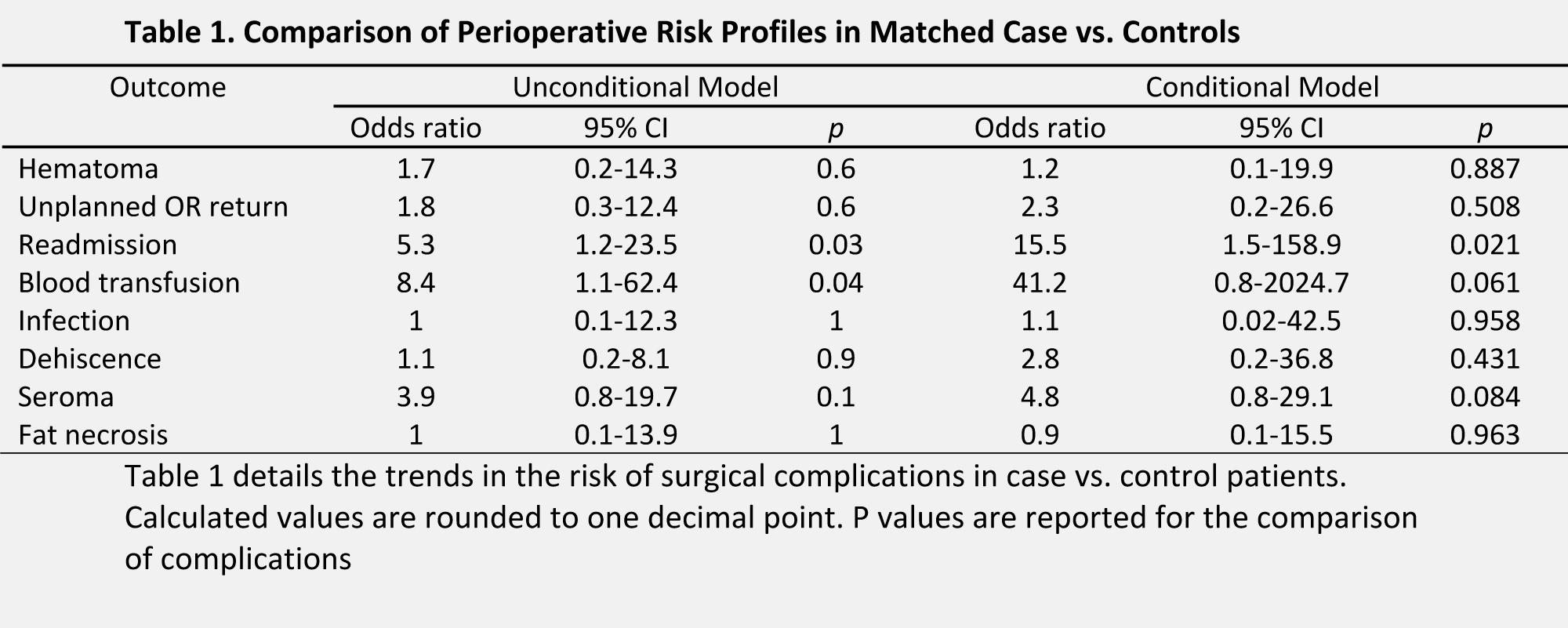
Results: A total of 1192 patients underwent abdominal contouring procedures, 19 (1.59%) experienced a postoperative venous thromboembolic event and were matched to 76 controls. The overall cohort was 92.6% female (n=88) with the average age, Charlson comorbidity index, BMI, and operative time being 44.99 year, 1.38 point, 30.25 units, and 284.69 minutes, respectively. Mean BMI differed significantly between cases and controls (32.1 vs. 29.8, p=0.046); and cases were more likely to have a prior history of cerebrovascular events (OR: 3.45, p=0.026). Additionally, patients with postoperative VTEs were more likely to have received intraoperative blood transfusions (OR: 13.88, p=0.005). Postoperatively, cases had significantly longer lengths of stay (6.21 vs. 1.21, p=0.006) and a much longer duration of chemophylaxis (6.05 vs. 1.46, p=0.015). Cases were significantly more likely to experience concurrent complications including infection, delayed wound healing, and umbilical necrosis (p<0.001, p=0.044, p=0.044 respectively). Plication was not associated with VTE outcomes.
Conclusion: This study demonstrates that abdominal plication does not increases the risk of VTEs after controlling for potentially predisposing factors via propensity score matching. However, in patients who do experience VTEs, further caution must be exercised as there is an increased likelihood of concurrent complications that may further complicate the postoperative course.
Back to 2022 Abstracts