The Impact Of Breast Cancer Type, Staging, And Treatment On Vascular Complications Of Free Flap Breast Reconstruction
Ankoor A. Talwar1, Dan Mazzaferro1, Martin Morris1, Harrison Davis1, Michael Hitchner1, Jared Shulkin1, Robyn B. Broach1, Ari Brooks1, Joseph M. Serletti1
1 University of Pennsylvania, Philadelphia, PA
Background: Patients with advanced cancer staging have a greater risk of developing venous thromboembolism (VTE) than no cancer alone. Approximately 1% of breast cancer patients experienced some form of VTE. The impact of breast cancer staging and treatment on clinical outcomes after autologous free-flap breast reconstruction (ABR) is not well-established. The objective of this retrospective study is to determine the impact of breast cancer characteristics, such as cancer staging, hormone receptor status, and history of VTE, on vascular complications of ABR.
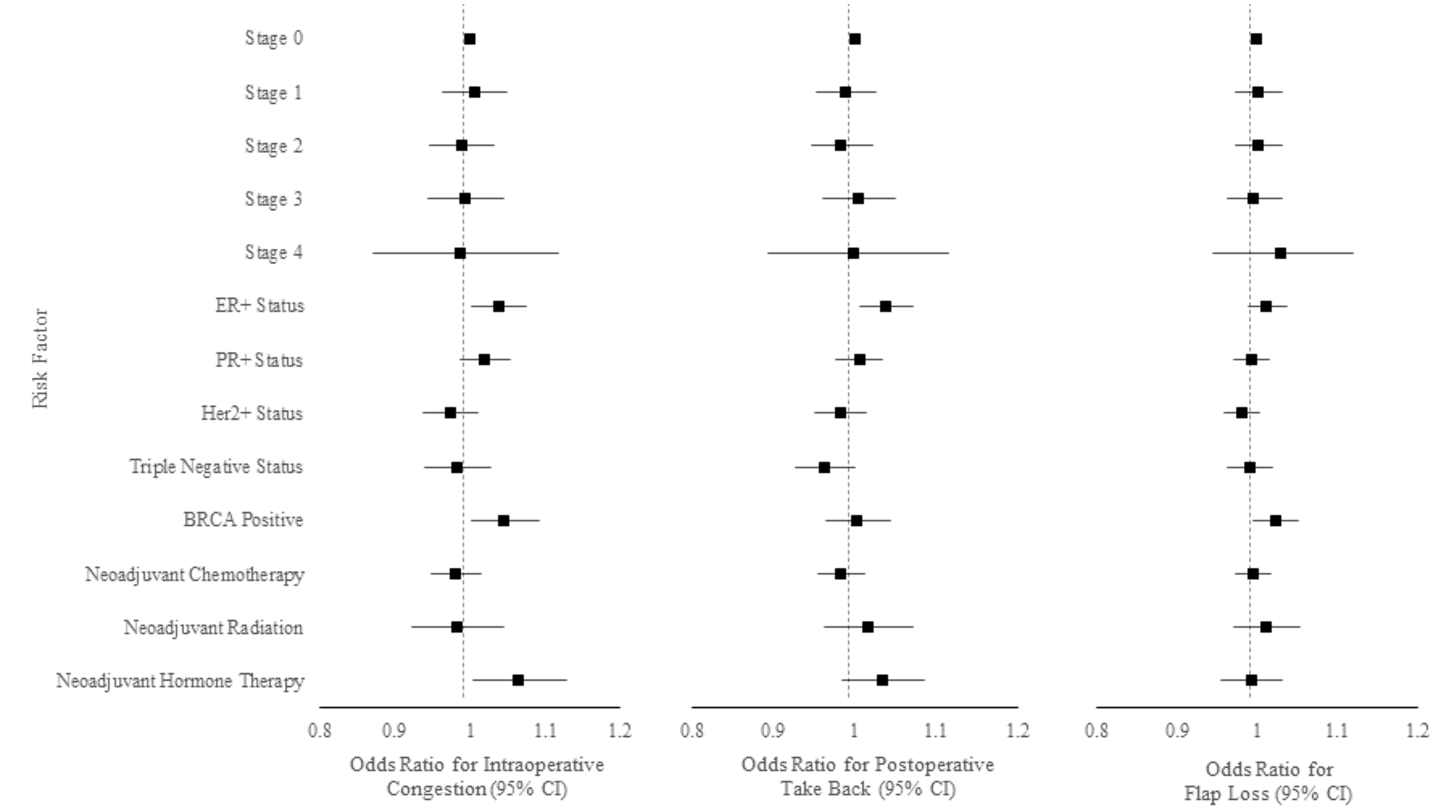
Methods: A retrospective review was conducted examining patients who underwent ABR from 2009-2018. Breast cancer staging, cancer types, hormone receptor status, and treatments were collected in addition to demographic data. Intraoperative and postoperative complications related to vascular compromise, including intraoperative congestion, postoperative take back for flap concern, and flap loss, were analyzed using a fixed effects logistic regression.
Results: 1,237 patients underwent free-flap ABR during the study period and were included. 12.7% of patients experienced a vascular complication following ABR (n=157), including 91 instances of intraoperative congestion (7.4%), 66 postoperative takebacks (5.3%), and 38 flap losses (3.1%). On fixed effect logistic regression, ER receptor positivity, BRCA positivity, and neoadjuvant hormone therapy were associated with intraoperative congestion (Figure). Only ER receptor positivity was associated with postoperative take back. No factor was associated with flap loss. In a sub-analysis of ER receptor-positive cancers, when adjusted for neoadjuvant hormone therapy, ER receptor positivity was no longer associated with intraoperative congestion, however it still was associated with postoperative take back (p<0.05). In a sub-analysis of Her2 receptor-positive cancers, treatment with Herceptin was protective against postoperative take back (p<0.05). Breast cancer staging, other hormone receptors, neoadjuvant chemotherapy, and neoadjuvant radiation were not individually associated with any vascular complications of ABR.
Conclusion: ER-positive and BRCA-positive breast cancer is a potential risk factor for vascular complications following autologous breast reconstruction. Neoadjuvant hormone and chemotherapy can affect risk of vascular complications. Breast cancer stage is not associated with increased free-flap vascular complications after ABR. Surgeons should factor breast cancer information into their clinical gestalt when providing ABR to patients. Patients should feel confident that, despite higher stage cancer, they can pursue their desired reconstructive option without fear of vascular compromise.
Back to 2022 Abstracts