Subclinical Skin Changes In Lymphedema Are Regional And Correlate With Both Dermal Backflow Patterns And Patient Reported Symptoms
Stav Brown, Adana Campbell, Joseph Dayan, Michelle Coriddi, Babak Mehrara
Plastic and Reconstructive Surgery Service, Department of Surgery, Memorial Sloan Kettering Cancer Center, New York, NY, United States.
Purpose: Lymphedema is a progressive disease that results from a compromised lymphatic system, often secondary to an iatrogenic injury during oncologic surgery. Fluid accumulation and stasis stimulate a series of pathological changes including inflammation, adipose tissue deposition, and soft tissue fibrosis which further impair lymph function. Despite their potential value in elucidating the pathophysiology of lymphedema development and potential role in detecting subclinical disease, current knowledge of early tissue changes in lymphedema is limited. The purpose of this study was to perform a preliminary analysis of the structural and functional skin alternations in early-stage lymphedema and evaluate their correlation with indocyanine green (ICG) lymphography findings and patient-reported symptoms.
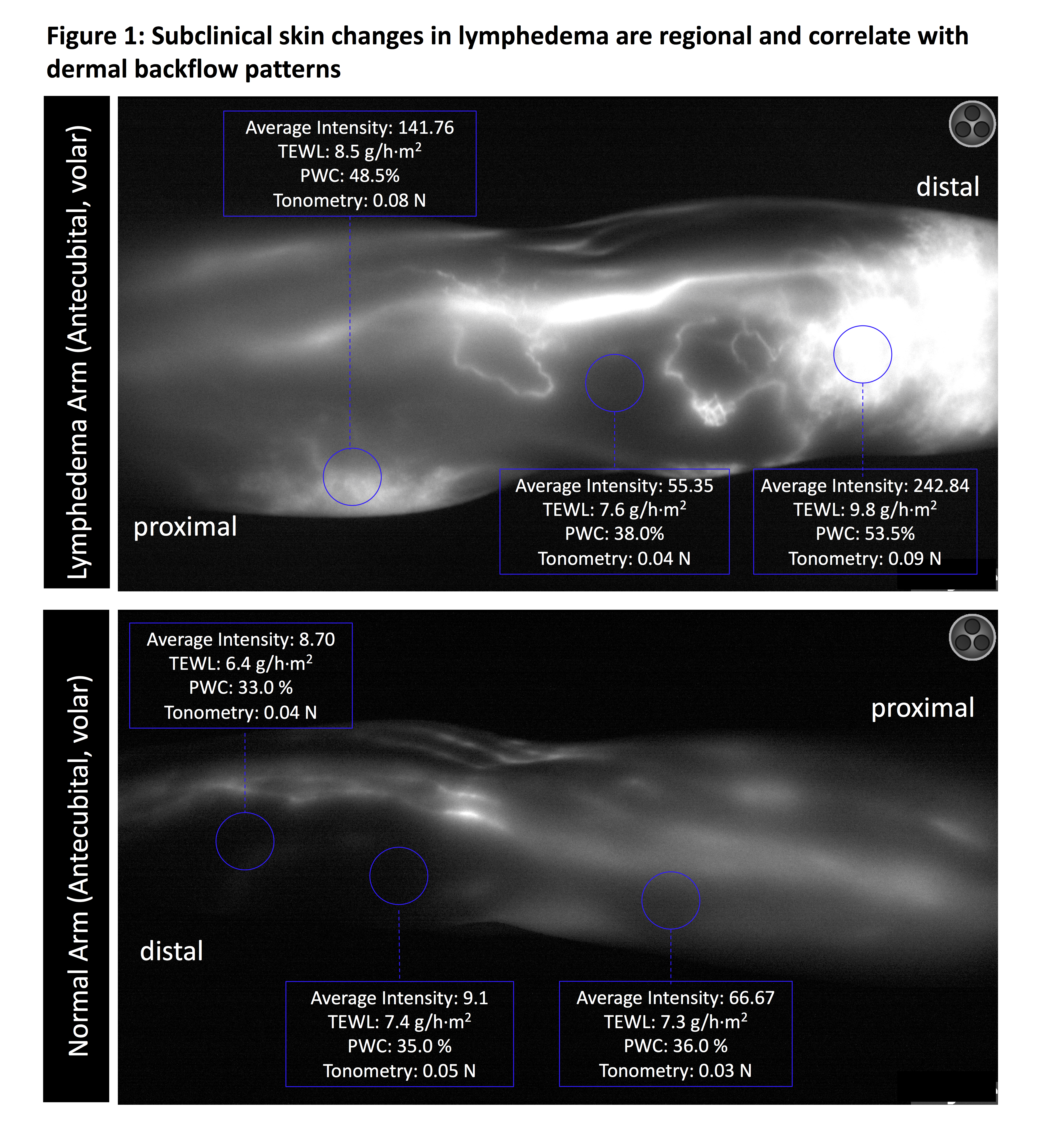
Methods: Trans-epidermal water loss (TEWL), tonometry (skin stiffness), and percentage water content (PWC) were measured in patients undergoing ICG lymphography using three non-invasive devices. Areas with the maximal dermal backflow in the volar upper arm and volar forearm, as well as a volar area not impacted by dermal backflow, were assessed. Respective skin sites of the contralateral limb were measured and used as controls. Each area was evaluated for average dermal backflow intensity quantified using Image J and patient-reported symptoms (scale 0-10, 0 means “no symptoms”). The Pearson coefficient was calculated to assess correlations between dermal backflow intensity skin measurements and symptom scores.
Results: Five patients with breast cancer-related lymphedema (BCRL) were included. Intensity of dermal ICG backflow was highly correlated with both TEWL (r=.73, p=0.0025) and PWC (r=.87, p<0.0001) and higher symptom scores (r=.92, p<0.0001). Higher TEWL values, indicating an impaired skin barrier function, were positively correlated with PWC (r=.86, p<0.0001) and tonometry (r=.64, p=0.01) values and higher symptom scores (r=.75, p=0.001). High correlations were found among PWC, TEWL, and tonometry.
Conclusion: Early-stage lymphedema is characterized by a localized increase in tissue water content, skin stiffness, and skin barrier dysfunction. These pathological skin changes are not uniformly distributed and are highly predictive of patient-reported symptoms and dermal backflow patterns on ICG. Early detection and quantification of localized skin alternations using simple, non-invasive methods applicable for clinical adaptation, could be a valuable complement in the screening and diagnosis of subclinical lymphedema, as well as a practical tool in the evaluation of responsiveness to treatments. These findings represent a major shift in current clinical practice paradigms, putting an emphasis on the prevention of disease progression rather than palliative treatments and symptomatic relief.
Back to 2022 Abstracts