Increased Access To Health Insurance And Rates Of Autologous Breast Reconstruction: Do State-Specific Trends Correlate To National Ones?
Ishani D. Premaratne MD 1, George S. Corpuz BA BS 2, Yoshiko Toyoda MD 3, Yuming Ning PhD 4, Paul Kurlansky MD 4, Christine H. Rohde MD MPH 4
1 Keck School of Medicine of the University of Southern California, Los Angeles, CA, USA 2 Weill Cornell Medicine, New York, NY, USA3 Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, USA4 Columbia University Vagelos College of Physicians and Surgeons, New York, NY, USA
Background: Health insurance disparities have been correlated to decreased access to surgical treatment for breast cancer. In 2014, states were given the option to expand Medicaid under the Affordable Care Act (ACA). The state-specific outcome of the Supreme Court ruling on Medicaid expansion provides a natural experiment to study its effects. It is unclear whether these trends are purely state-specific or representative of the national impact of this sweeping healthcare policy. Given the importance of insurance on health outcomes and the benefits of breast reconstruction, we sought to understand whether the state experience could be generalized to a national one.
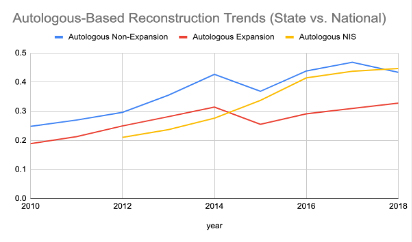
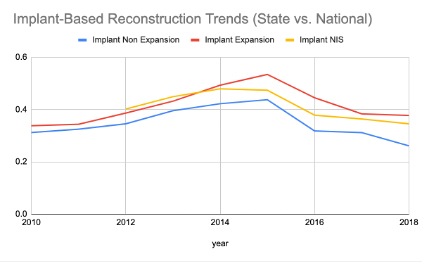
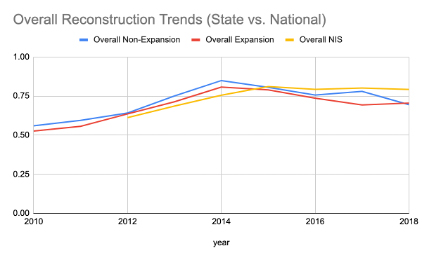
Methods: Seven expansion and six non-expansion states were selected. The Health Care Utilization Project (HCUP)-State Inpatient Data was queried for breast reconstruction rates (autologous and implant-based) from 2010-2018. A difference-in-difference linear mixed model was utilized to compare breast reconstruction rates between expansion and non-expansion states before and after 2014. We then used trend analysis to compare state-based reconstruction trends to the HCUP-National Inpatient Sample.Results: From 2010-2018, change in overall rates of insurance coverage after Medicaid expansion was statistically greater in expansion than non-expansion states (p=0.001). Independently, the increase in autologous reconstruction rate was statistically greater in expansion vs. non-expansion states (p=0.0098), while the increase in implant-based reconstruction rate was not. There was therefore no significant change in overall breast reconstruction rate (both autologous and implant-based) after Medicaid expansion in states that expanded Medicaid. Regarding autologous reconstruction, national and state-specific trends were significantly different (in both expansion and non-expansion states). For implant-based reconstruction, only trends in non-expansion states were significantly different from national trends (while trends in expansion states aligned with national trends). Finally, regarding overall reconstruction trends, national trends aligned with both expansion and non-expansion state trends.
Conclusions: We update prior findings with extended data from 2010-2018. When comparing expansion to non-expansion states with a difference-in-difference model in terms of autologous and implant-based reconstruction rates, the decision to expand Medicaid in 2014 is correlated with a significant increase in autologous, but not implant-based breast reconstruction rates. Further study is required to elucidate which factors have influenced patients who newly gained insurance under the ACA’s Medicaid Expansion provision to favor autologous over implant-based reconstruction. When comparing expansion and non-expansion state-based trends to national trends, we find that national trends do correlate with implant-based reconstruction rates in expansion states as well as overall reconstruction rates in both expansion and non-expansion states.
Back to 2022 Abstracts