Flap Coverage of Infected Ventricular Assist Devices Influences Patient Outcomes
Keith Sweitzer, MD1 James Butterfield, MD1, Megan Pencek, MD1, Jessica Huber, BS1, Won Park, BS1, Julia Tomtschik, BS1 Mathew Carter, BS1 Savannah Russ1 ,MS Derek Bell, MD1
1University of Rochester, Department of Surgery, Division of Plastic Surgery, Rochester, NY;University of Rochester Department Epidemiology, Rochester, NY
Background: The use of ventricular assist devices (LVADs) for patients with end-stage cardiac failure awaiting heart transplantation has become increasingly common. VADs improve the longevity and the quality of life for these patients and serve as a bridge to cardiac allograft transplantation. However, ventricular assist device-related infections remain a major problem complicating their long-term use. As these are life-sustaining devices, simple explanation is often difficult, or directly impossible. Clinical infection and sepsis can critically threaten these patients with ventricular assist devices.
Methods: Patients who underwent insertion of a ventricular assist device and had a subsequent readmission for LVAD infection at the University of Rochester Medical Center from 2012-2022 were identified through accessing the medical records archives of the hospital. Patients were followed retrospectively for an average of 3.2 years. Review of patients' medical records was conducted to obtain patient demographics, preoperative diagnosis and disease state, type of ventricular assist device inserted, postoperative day of ventricular assist device infection onset, infectious organism identified at initial washout, infectious organism identified at time of definitive device coverage, timing of coverage procedure after the initial washout for infection, type of flap used for coverage, 90 day complications following definitive coverage and lifetime return to OR for infection. Comparison analysis with a Chi squared test was used to analyze outcomes.
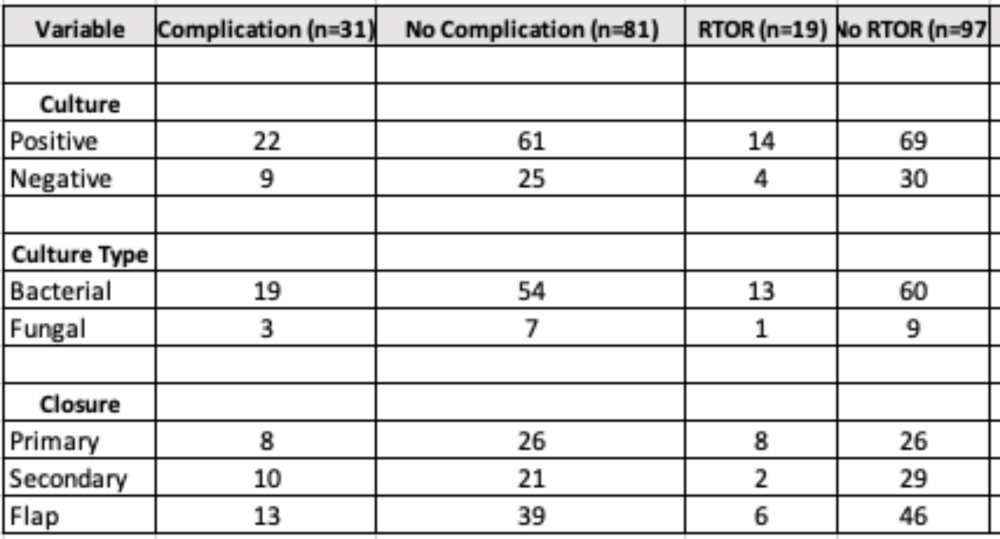
Results: Of 568 patients admitted with an LVAD related infection 117 underwent operative debridement. Of these, 34 underwent primary closure, 31 underwent closure with secondary intention (NPWT with STSG), and 52 were closed with a flap (pectoralis, omental, latissimus, or VRAM). There was a statistically significant higher incidence of RTOR for infection over a lifetime with primary closure compared to secondary intention and flap reconstruction (p=0.01,0.02), but no difference in 90 day complications (p=0.76, p=0.58). 83 patients had a positive culture upon definitive coverage with 24 having a post surgical complication, 15 of which required RTOR for infection. 34 were closed with negative cultures with 9 having a complication, and 4 requiring RTOR for infection. This was not statistically significant for complications or RTOR (p=0.79, 0.40). Culture data was further sub-stratified into bacterial cultures (n=73) vs fungal cultures (n=10) there was no statistically significant difference between these compared to complications or RTOR (p=0.40, 0.39)
Conclusion: Coverage of infected LVADs with loco-regional flaps or allowing to granulate using wound vac therapy with future STSG has a decreased lifetime RTOR for future infections for these patients.
Back to 2022 Abstracts