Socioeconomic Status and Treatment Delays in Non-Syndromic Craniosynostosis: A 30-Year Retrospective Case-Control Analysis on Gaps to Care
Isabel V Lake1, Christopher D Lopez1, Alexander K Karius1, Ava Niknahad1, Kimberly H Khoo1, Alisa O Girard1, Richard J Redett1, Robin Yang1
1 Department of Plastic and Reconstructive Surgery, Johns Hopkins University School of Medicine, Baltimore, MD.
Background: Patients with non-syndromic craniosynostosis (NSC) generally undergo corrective surgery before one year of age to the mitigate morbidities of delayed surgery, including greater operative times, increased rate of residual skull defects, and prolonged risk of brain growth restriction. Though the number of patients who undergo primary correction for NSC after this optimal one-year window is not insignificant, this cohort, as well as the factors associated with their gaps to care, are poorly characterized in literature.
Methods: A 30-year retrospective case-control study was conducted for all NSC patients who underwent primary corrective surgery at our institution and its affiliates between 1992-2022. Patients whose surgery occurred after one year of age were identified and matched 1:1 by surgical date to standard care controls whose surgery occurred prior to one year of age. Chart review was conducted to gather data regarding care timeline and sociodemographic characteristics for all patients. Comparative statistics and bivariate regression were used to assess the impact of these characteristics on care delays.
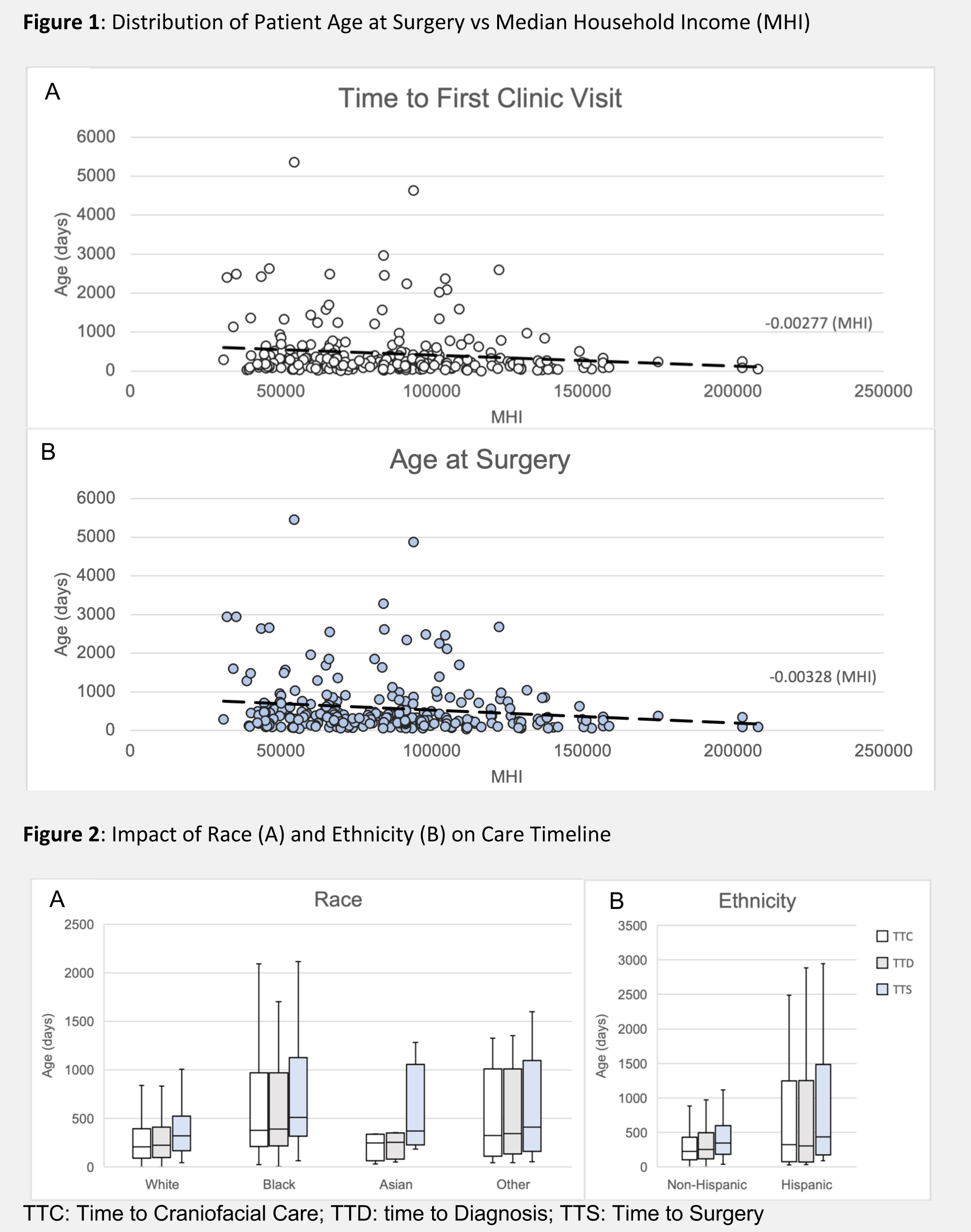
Results: Odds of surgical delay (>12 months of age at repair) were increased in patients who were of Black race (OR: 3.56, p<0.001), insured by MCOs (OR: 2.56, p=0.029), lived with single caregivers (OR: 6.13, p=0.005), and were from lower income households (1.4% increase in risk of delay per $1000 decrease in MHI, p<0.001). Lack of timely access to an appropriate craniofacial provider was primarily responsible for surgical delays seen in patients of Black race (342-day provider delay and 391-day surgical delay, p=0.001 and <0.001), with MCO insurance (274 and 378 days, p=0.033 and 0.008), with immigrant parent(s) (1486 and 1543 days, p<0.001 for both), and from low-income households (2.8 and 3.3 day delays per $1000 decrease in MHI; p=0.031 and 0.017). Oppositely, Hispanic ethnicity and language barriers led to delays receiving timely correction following establishment of appropriate care (119-day and 132-day delays in diagnosis-to-surgery interval, respectively, p=0.017 and 0.014). Parental strain was implicated in delays across all timepoints, especially for patients whose parental status was associated with tenuous or volatile access to care.
Conclusions: NSC patients from households experiencing socioeconomic and familial strain face systemic barriers to adequate care access. Further, the necessarily compressed timeline of care for craniosynostosis patients magnifies disparities in surgical outcome resulting from these delays. Interventions both at primary care and craniofacial specialist levels are necessary to decrease health care gaps and optimize outcomes for vulnerable patients.
Back to 2022 Abstracts