Non-Implant-Based Methods for Gluteal Augmentation: A Systematic Review on Best Techniques and Reported Outcomes
Tristan H. Wesson1, Rafael Felix P. Tiongco1, Alisa O. Girard1, Alexander K Karius1,Amanda L. Chow2, Alice L. Zhou1, Joseph S. Puthumana1, Stella M. Seal1, Carisa M. Cooney1, Kristen P. Broderick1
1Department of Plastic and Reconstructive Surgery, The Johns Hopkins University School of Medicine, Baltimore, MD2Division of Plastic and Reconstructive Surgery, Rutgers New Jersey Medical School, Newark, N
Background: In 2018, the American Society of Plastic Surgeons estimated the death rate for gluteal fat transfers, also known as “Brazilian butt lifts,” at 1 in 3,000. This is the highest death rate for any cosmetic procedure and many are performed by non-board certified plastic surgeons. We therefore conducted a systematic review with goals of elucidating: (1) the published non-implant based techniques for gluteal augmentation, (2) associated complications, and (3) providers performing these procedures.
Methods: We conducted a systematic review under PRISMA guidelines. PubMed, Embase, Cochrane, Web of Science, Scopus, and ClinicalTrials.gov were queried for studies in English with original data on non-implant based procedures for cosmetic gluteal augmentation. Massive weight loss patients and patients with congenital deformities or trauma were excluded. Demographic, intraoperative, complications, and provider data were extracted.
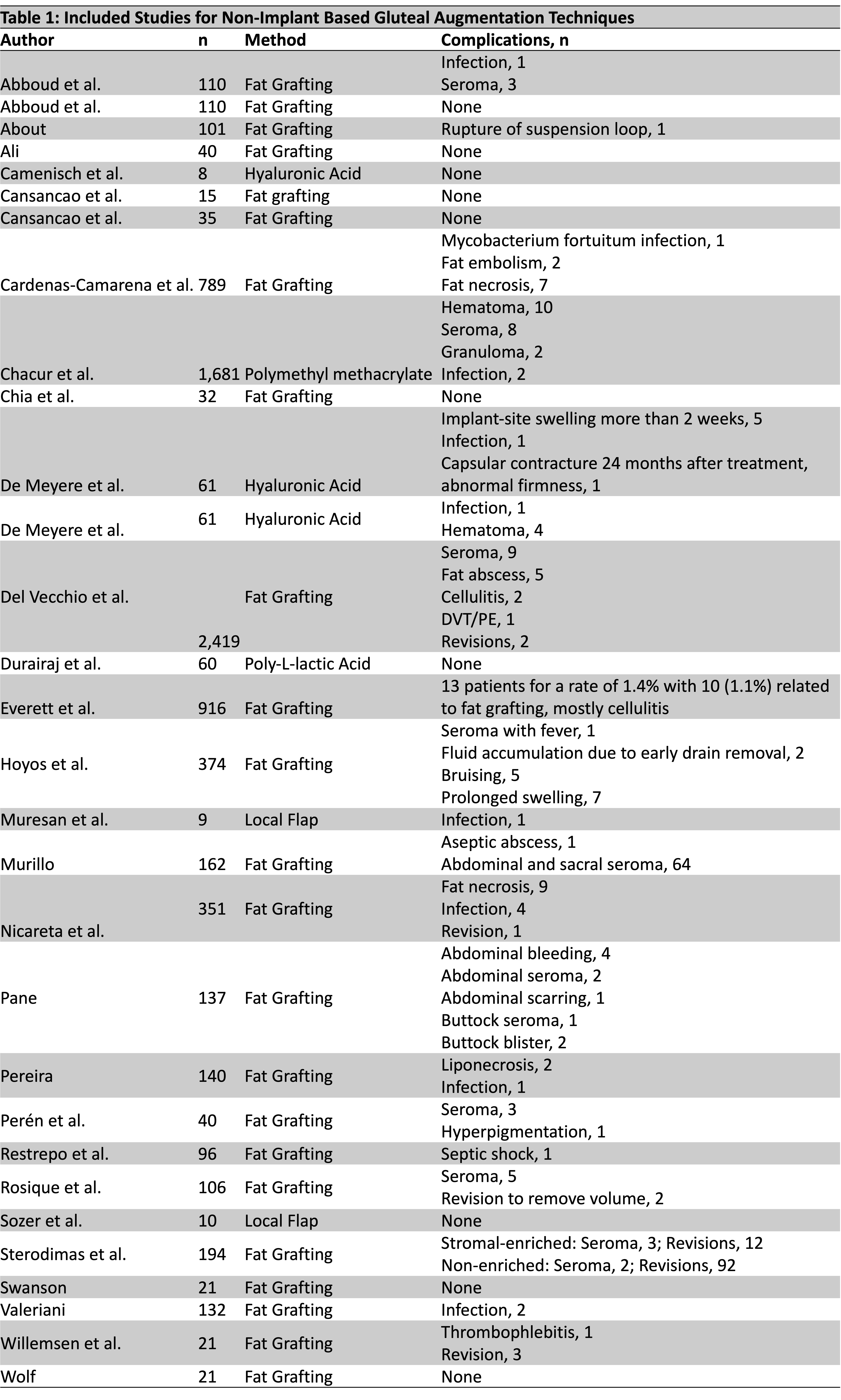
Results: Of 4188 articles identified, we included 30 studies included from 9 countries (Table 1). A total of 8252 patients (93.3% female and 6.7% male) aged 17 to 76 years old underwent gluteal augmentation via fat grafting (77.1%), biopolymer filler injection (22.7%), or local flap (0.2%). All procedures were performed by plastic surgeons board-certified in their countries. Intramuscular injections were explicitly mentioned by 20.0% of studies but not since 2010. Volumes of fat injected per buttock ranged from 100 to 2200 ccs. Follow-up time ranged from 0.2 to 144 months. Complications included infections (0.3%), hematoma/seroma (0.6%), fat necrosis (0.2%), DVT/PE (n=1), septic shock (n=1), fat embolism syndrome (n=2).Though not included due to small sample sizes, there were 56 studies reporting morbidity and mortality including case reports (n=81.9%), case series (n=14.5%), and autopsies (n=3.6%). Methods included fat grafting (30.9%), non-medical grade liquid silicone (43.6%), or other substances (25.5%) performed by unknown means or unlicensed practitioners (90.9%), plastic surgeons (5.5%), or other medical specialties (3.6%). Death was reported in 10.7% of studies due to fat embolism syndrome with evidence of gluteal vessel laceration on autopsy. Women (71.9%) represented the majority of injured patients followed by transgender individuals (25.5%) and men (2.6%).
Conclusions: Our systematic review summarizes available published surgical techniques and outcomes from board-certified plastic surgeons for non-implant based gluteal augmentation. Surgeons with board certification in plastic and reconstructive surgery provide the safest outcomes. The most serious of these complications, such as mortality, life-threatening infection, and embolic events are not described as robustly in the plastic and reconstructive literature, but are instead reported in case reports and autopsies.
Back to 2022 Posters