Comparison of TMR vs. RPNI for Mitigation of Post-Amputation Residual Limb Pain
Corey Bascone1, Reena Sulkar2, Robyn Broach3, Scott Levin4, Stephen Kovach5
University of Pennsylvania, Department of Surgery Division of Plastic Surgery, Philadelphia, PA USA
Background: Targeted Muscle Reinnervation (TMR) and Regenerative Peripheral Nerve Interfaces (RPNI) have both been implemented in lower extremity amputations, as a means of preventing postoperative residual limb pain (RLP) associated with neuroma formation. This study seeks to compare the frequency of RLP in nerves prepared using TMR or RPNI in patients undergoing below-knee amputation (BKA).
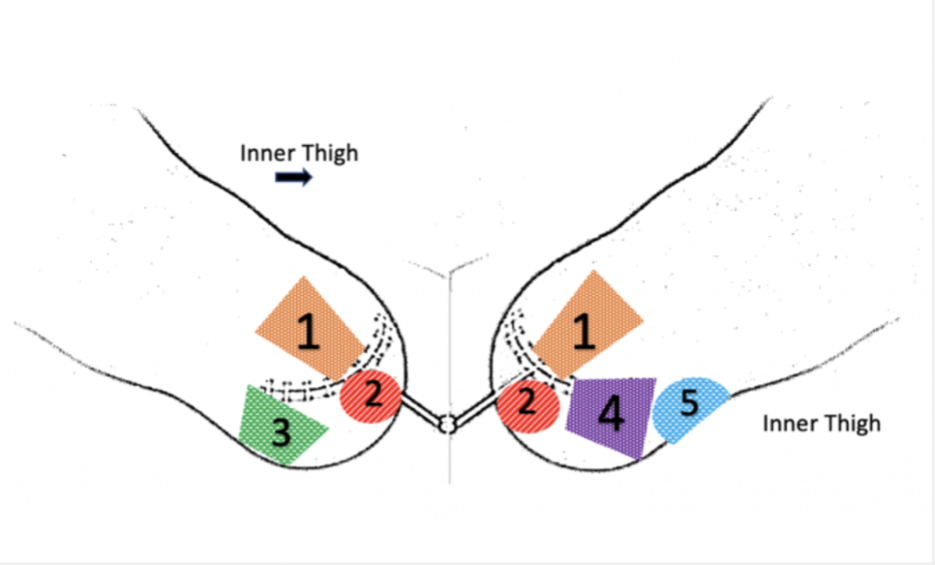
Methods: A single surgeon’s case log over two years at the University of Pennsylvania were used to identify patients who underwent a BKA with neurotized lateral compartment flap, with 90 days of follow up. An online survey and interactive diagram was sent to 25 eligible patients in order to assess patient-reported RLP and phantom limb pain (PLP). Operative reports were retrospectively reviewed for data on the nerve preparation techniques utilized.
Results: A total of 21 participants (15 males, 6 females) responded (84% response rate). The mean age of respondents was 52. 76% (n=16) suffered from diabetes mellitus, 48% (n=10) had vascular disease, and 57% (n=12) were current or former smokers. The average time from surgery to survey response was 461 days. Two patients were excluded from further analysis after indicating active wounds on their residual limb. Of 19 remaining respondents’, twelve had no pain at all (63%) and just seven reported RLP (36.8%). Only five patients who were surveyed reported phantom limb pain (PLP) (29.4%). 75% of the respondents with no RLP at all were diabetics. Among the seven individuals who reported RLP, several indicated multiple regions on the diagram as the causation of their pain. Most regions contained a nerve prepared with a RPNI (50%), five contained a nerve prepared with TMR (31.25%), and the rest were derived from regions where the nerve could not be found intra-operatively (18.75%). The nerves responsible for the highest pain category were the deep peroneal nerve (35%), followed by the posterior tibial nerve (21.4%), and the sural nerve (21.4%). The region containing the superficial peroneal nerve was indicated as highly painful twice (14.3%), and the saphenous nerve was indicated once (7.1%).
Conclusions: When considering lower limb reconstruction, utilizing a neurotized lateral compartment flap with a combination of TMR or RPNI successfully mitigates postoperative pain, even in the diabetic population. Due to patient-reported ‘high pain regions’ most often containing nerves prepared with RPNIs, TMR and additional techniques that protect the coaptation from axonal escape should be considered primarily, especially in large caliber nerves.
Back to 2022 Posters