Machine Learning to Determine Factors Influencing Cranial Index Following Spring Mediated Cranial Vault Expansion in Non-Syndromic Sagittal Craniosynostosis
Dillan F Villavisanis1,2, Sameer Shakir1, Daniel Y Cho1, Chao Zhao3, Carlos Barrero1, Jessica D Blum1, Jordan W Swanson1, Scott P Bartlett1, Alexander M Tucker2, Jesse A Taylor MD1
1Division of Plastic & Reconstructive Surgery, Children's Hospital of Philadelphia, Philadelphia, PA, USA2Division of Neurosurgery, Children's Hospital of Philadelphia, Philadelphia, PA, USA3Center for Data Driven Discovery in Medicine, Children's Hospital of Philadelphia, PA, USA
Introduction: Spring-mediated cranial vault expansion (SMC) is an increasingly utilized tool in non-syndromic sagittal craniosynostosis but variables impacting outcomes, including bone thickness, are incompletely understood. The aim of this study was to determine variables that interact to predict SMC outcomes, primarily changes in cranial index (CI).
Methods: Patients with non-syndromic sagittal craniosynostosis undergoing SMC at our institution between 2014 and 2021 were included. Clinical data, including CI over time (immediately postoperative; one, three, six months; and one, three, and five years postoperative), were obtained from patient medical records. Skull thickness was determined in from patient preoperative CTs in Materalise Mimics. Stepwise selection, least absolute shrinkage and selection operator (LASSO), and random forest machine learning methods were used to determine variables most predictive of changes in CI.
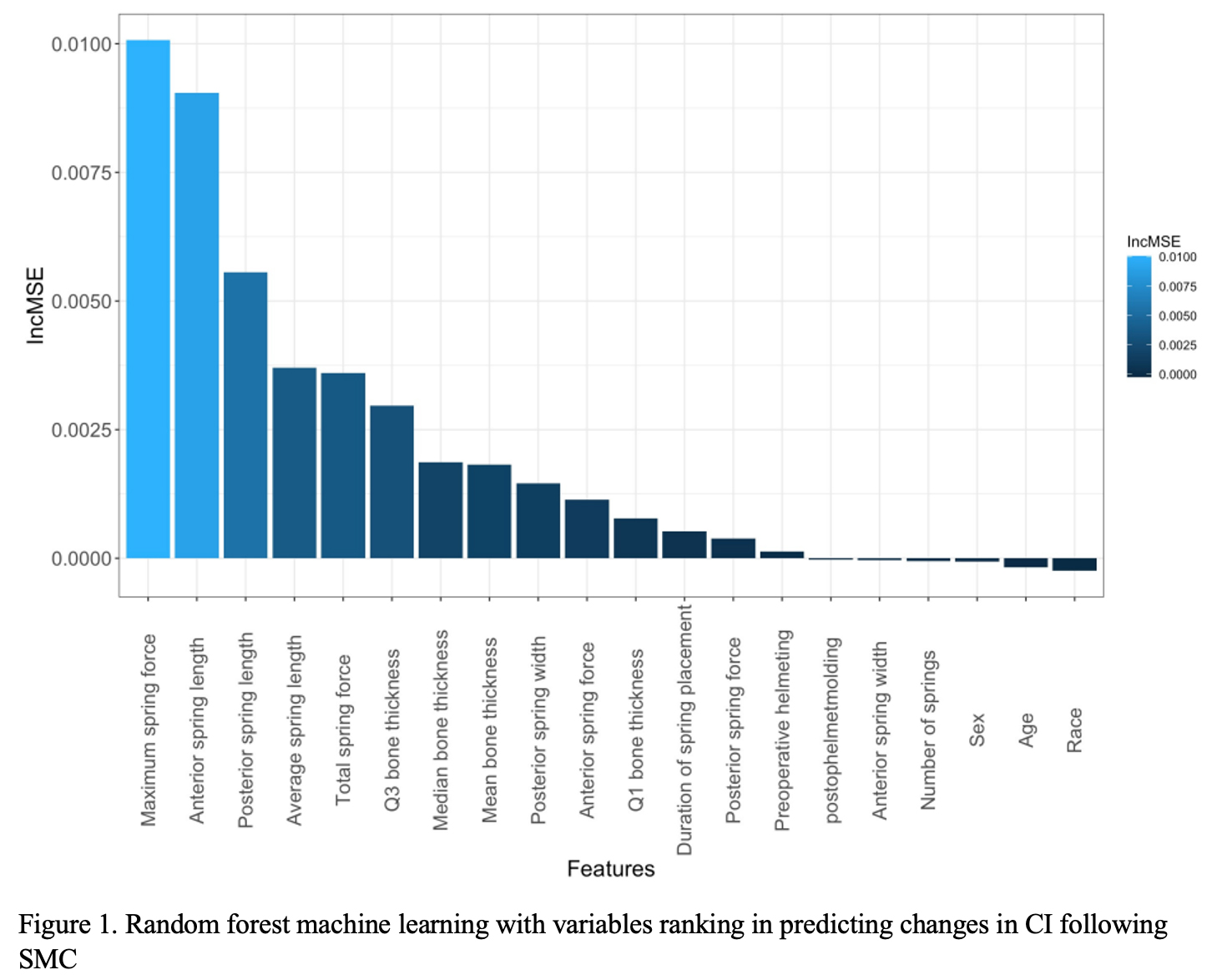
Results: One hundred and twenty-four patients (94 males) with mean surgery age of 3.59 ± 0.87 months and average skull thickness 1.83 ± 0.38 cm were included in this study. Random forest machine learning identified maximum spring force and mean thickness as highly predictive variables with increased in mean squared error (IncMSE) as 0.0173 and 0.0136, respectively, and more predictive than sex (0.0013) and age at surgery (-0.0004). In stepwise analysis, maximum spring force (? = 0.108, CI = 0.056 – 0.161, p < 0.001), anterior spring force (? = 0.052, CI = -0.097 – -0.006, p = 0.027), and duration of spring placement (? = 0.002, CI = 0.000 – 0.003, p = 0.046) best predicted changes in CI, and LASSO analysis identified the same three variables as most predictive (? = 0.027, -0.006, 0.0005, respectively).
Conclusions: This study demonstrates maximum spring force, duration of spring placement, and parietal bone thickness may be good predictors of CI changes in patients undergoing SMC. Age at surgery and other demographic variables were inferior predictors in models using our cohort.
Back to 2022 Posters