Amputation Acceptance: A Survey of Factors Influencing the Decision to Undergo Lower Extremity Amputation
Gina Cach BA1, Ashley E. Rogers MD2, Daisy Spoer MS1, Adaah A. Sayyed BS1, Romina Deldar MD2, Christopher E. Attinger MD2, Karen K. Evans MD2
1. Georgetown University School of Medicine, Washington, DC2. Department of Plastic and Reconstructive Surgery, MedStar Georgetown University Hospital, Washington, DC
Background: Losing a limb redefines a patient’s identity and functionality. Undergoing amputation is often fraught with confusion, fear, and uncertainty. To assess the most effective methods to facilitate discussions about amputation with at-risk patients, we surveyed lower extremity (LE) amputees treated at a tertiary limb salvage center regarding this decision-making process.
Methods: Following IRB approval, patients who underwent LE amputation at MedStar Georgetown University Hospital from October 2020 to October 2021 were asked to complete a five-item phone survey assessing their decision to undergo amputation and their overall satisfaction after the procedure. Patient demographics, comorbidities, operative details, and complications were collected using electronic medical records.
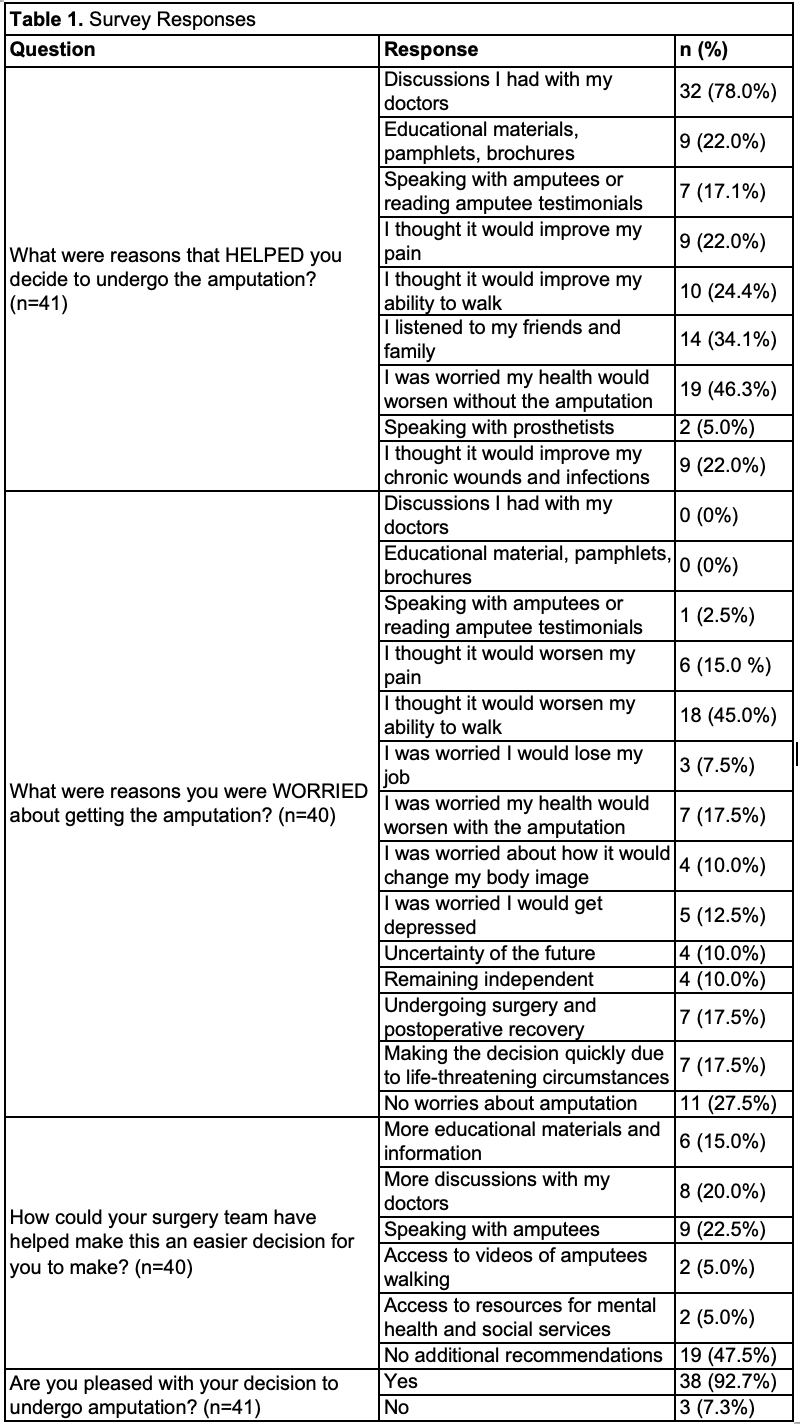
Results: Of 89 LE amputees identified, 41 (46.1%) responded to the survey. Mean age and body mass index were 59.7±15.5 years and 31.7±7.0 kg/m2, respectively, with a mean Charlson Comorbidity Index score of 5.4±2.7. The most common indications for LE amputation were infection (n=22, 53.6%) and ischemia (n=9, 21.9%). Most patients underwent below-knee amputations (n=34, 82.9%) and received targeted muscle reinnervation (TMR; n=30, 73.2%) or regenerative peripheral nerve interface (RPNI; n=7, 17.1%). Post-operative complications included dehiscence (n=5, 12.2%) and infection (n=3, 7.3%). At a mean follow-up of 5.9±3.5 months, 20 patients (48.8%) were ambulatory. Surveys were completed at a mean of 7.7±4.0 months since amputation. Reasons that helped patients decide to undergo LE amputation included discussions with doctors (n=32, 78.0%), concern for worsening health without amputation (n=19, 46.3%), and advice from friends and family (n=14, 34.1%). Worsening ability to walk after amputation (n=18, 45.0%) was the most common concern. Other concerns included deteriorating health (n=7, 17.5%), surgery itself and postoperative recovery (n=7, 17.5%), and having to make the decision quickly due to life-threatening circumstances (n=7, 17.5%). However, 11 patients (27.5%) reported no concerns with undergoing amputation. When asked about ways the surgical team could have eased the decision-making process, many had no recommendations (n=19, 47.5%); however, 22.5% (n=9) stated that speaking with other amputees would have been helpful. Most patients were pleased with their decision to undergo amputation (n=38, 92.7%).
Conclusion: Patients primarily cited satisfaction with their decision to undergo LE amputation and that they would not recommend changes to the decision-making process. Using functional-based amputations and pain reduction techniques (i.e., TMR or RPNI) may have impacted our patient population to provide satisfying postoperative results. Nevertheless, it is critical to consider factors affecting these decisions and incorporate patient recommendations to improve the decision-making process.
Back to 2022 Posters